Where is the sphincter?
Fundamental misconceptions about the lower esophageal sphincter (LES) pervade
the literature of manometry.
It is widely believed there is a subphrenic esophageal segment that contains
the sphincter.
It is also believed that intraabdominal pressure "backs up" the physiologic
sphincter rendering it competent(1) Such statements
imply that their authors believe the sphincter is in this subphrenic segment.
It is believed to be 2.5 cm or more in length.
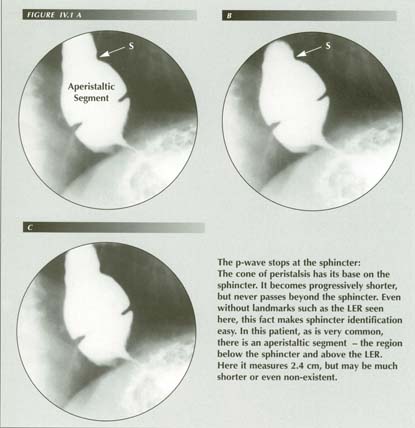
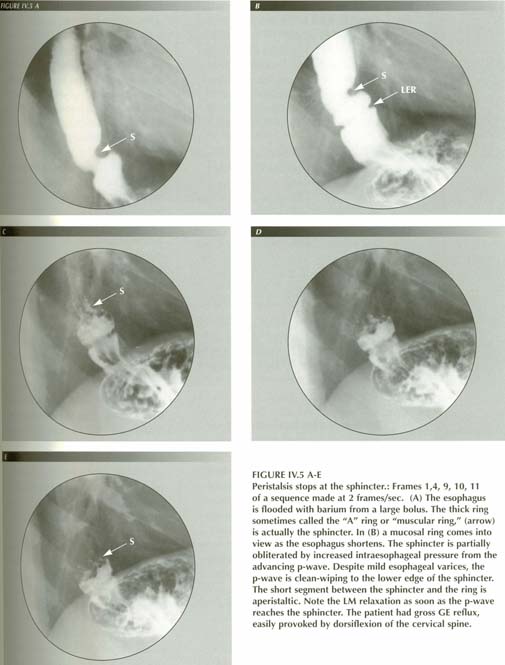
Unfortunately, these beliefs provide the rationale for antireflux surgical procedures. It is equally unfortunate that the actual sphincter described and named by Lerche(2), that is plainly visible radiologically, has been misinterpreted(3) and even described as an obstructive lesion similar to the LER.(4) Radiologically, there is no difficulty in locating the normal sphincter: it is at the end of the peristaltic wave. The peristaltic wave does not pass through the diaphragm. Hence there could hardly be a subphrenic segment of esophagus.
As the PEL in inserted at the sphincter, the sphincter will be above the diaphragm
in a patient with normal LM tone. In a sense the sphincter is the stationary
end of the peristaltic wave. There is no peristalsis in the fundus of the stomach
or distal to the sphincter in the .3-3 cm aperistaltic esophageal segment interposed
between the sphincter and the fundus.
The manometric data are detailed, pervasive and hazardous to challenge as
they are backed by immense authority. It has been done, however, although the
work has been successfully ignored. In 1985 Clark(5)
resected the sphincter area and replaced it with a tube of jejunum or colon
in 12 Rhesus monkeys. Remarkably, a high pressure zone (HPZ) was recorded
on 89.6% of the manometer tracings after jejunal interposition! Even the
pattern of "receptive relaxation" during the pharyngeal phase of swallowing
was recorded in many. Moreover, some of the reported pharmacological effects
on the sphincter were reproduced in these animals. Clark concluded that ". .
. the HPZ resulted mainly from compression of the bulky jejunum as it passed
through the oblique right crus of the diaphragm."
Clark's criticism of the HPZ location of the LES is well taken and may explain the belief in a subphrenic sphincter. The manometer must be recording a squeeze of the fundus in the hiatus. This was demonstrated unintentionally by a study in which the GE junction area was simultaneously recorded by both cineradiography and manometry in 13 patients with lower esophageal rings (LER).(6) The HPZ was found to lie below the LER. In rigid conformity with manometric doctrine, the authors were forced to conclude that, "The lower esophageal ring was found at the proximal margin of the lower esophageal sphincter in all [13] patients."
As the number of pathological examinations of LER's increases, it becomes
impossible to maintain that the LER is not exactly at the junction of squamous
and glandular mucosa. The above finding can only have one interpretation: the
HPZ the manometer was recording was in the stomach! Examination of the reproduced
cine frames shows this to be the case. Metal tipped catheters are 2.5-3 cm into
a hiatus hernia and hence subject to a hiatal squeeze.
If manometry places the HPZ about 2.5 cm distal to the true GE junction, i.e.
in the stomach, 100% of the time in 13 patients, we have an explanation for
the manometric inference of a subdiaphragmatic esophagus: the low resolving
power of the manometer could easily misplace it.
It is interesting to note in Clark's report that all of the familiar "sphincter"
phenomena - reduced pressure with deglutition, pharmacologic effect of propantheline,
etc. - were present at the HPZ after extirpation of the sphincter!
Clark advances this as evidence that there is no LES, but it also demonstrates
that something will lessen the "squeeze" pressure being measured at
the HPZ whether or not it is acting on a sphincter. That something, it will
be shown, is the LM. The pharmacological effects, etc. could be equally well
be due to action of the drug on the LM.
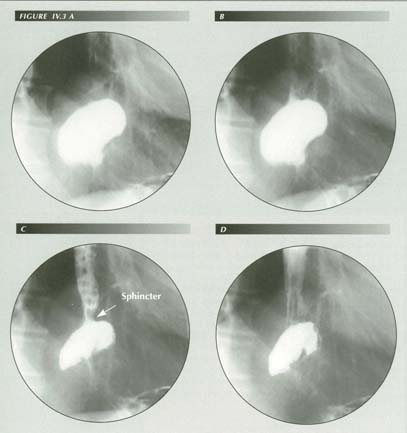
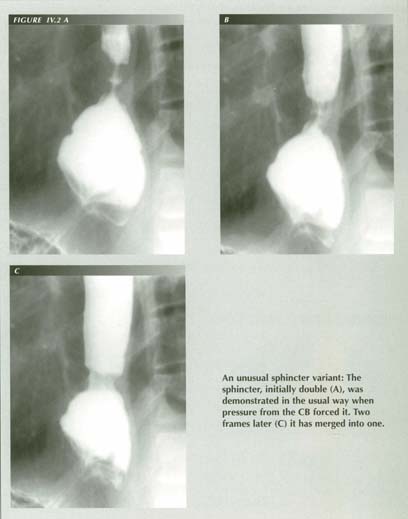
The lower esophageal sphincter: Here the bulb-sryringe action of mesentery crowding into the tented PEL is powerful enough to override the sphincter, forcing the captive bolus back into the body of the esphagus. At this instant, the true length of the sphincter is seen to be only 7-8 mm - far shorter than has been supposed from the evidence of manometry. The sphincter remains closed against this considerable force from below, but when it does yield (after 3 seconds) it then relaxes completely within a second. Gastric mesentery crowded into the PEL tent by the Valsalva maneuver is the driving force.
If , for example, one were to loop a cord around the a hollow organ as an external
constraint, traction on the cord would press on only one side of the lumen.
The organ would move laterally until constrained by equal pressure from the
opposite side. On the other two sides the pressure would be intermediate. Intraluminal
readings would vary depending on where pressure was being measured. What is
this external constraint? It could only be the hiatal ring.
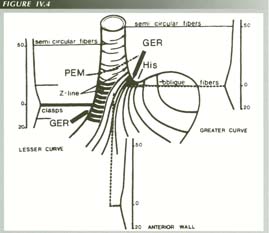
Synthesis. The site of muscular thickness, muscle fiber arrangement. PEM, and Z-line are related to each other.
Figure 12 from Liebermann-Meffert, D. et al., Muscular equivalent of the lower esophageal sphincter, Gastroenterology 76:32-8, 1979 Used with permission.
Liebermann-Meffert and her collaborators,(9),(10)
perhaps because of their exacting technical methods, have had the last word
as far as anatomical sphincters in the region. They described a gastroesophageal
ring (GER) of circular smooth muscle 16.4 mm' below the descending limb of the
PEL. The ring was 4.2 mm thick on the greater curvature side and a mm less on
the lesser curvature side. It tapered up into the normal esophageal CM thickness
of 2.1 mm over a distance of about 5 cm but tapered more abruptly distally.
It was asymmetrically higher on the greater curvature side. [See their Figure
12]
As can be seen from their figure, the fibers do not run circularly but consist
of short clasp-like fibers on the lesser curvature side and oblique, almost
longitudinal, fibers on the greater curvature side. The axial length of the
thickening was determined to be 2.3 cm on the lesser curvature side and 3.1
cm on the greater curvature, but because of the tapering, it is difficult to
define the end points.
It is difficult to see what significance should be attached to this GER but
the suggestion that it represents the physiologic LES must be refuted. It is
9-21 mm below the ora serrata. [We must recall that the mucosal LER
is here.] It is even farther below the PEL. If all of its fibers were to contract
simultaneously, they would produce a distortion of the GE junction, but not
the annular constriction required for sphincter function.
It has, nevertheless, been widely accepted as the anatomical counterpart of the physiologic sphincter as defined by manometry. The acceptance derives from the fact that manometry also assigns a 3-5 cm length to the physiologic sphincter and locates it below the diaphragm, well below the PEL. This places it below the aperistaltic segment that can be demonstrated radiologically between the sphincter and the ora serrata. As this has a length of .3 to 2.5 cm, the Libermann-Meffert muscle thickening is 1.4 to 4.6 cm below the lower edge of the radiological LES - that is, well below the endpoint of the peristaltic wave and clearly in the stomach.
I cannot find any justification for supposing that the physiologic sphincter
of the esophagus is in the stomach and in a region quite devoid of peristaltic
activity. It is in an area that, if above the diaphragm, would be a HH!
The Libermann-Meffert GER does not make sense in physiological terms. It is
physiologically and logically imperative that the p-wave pass uninterruptedly
to the sphincter - passing the baton, so to speak. If there were a gap, the
bolus would be lost and reflux would occur back into the body of the esophagus
as soon as the advancing ring of circular muscle contraction stopped and died
out.
The p-wave does stop. It then either dies out or it does not. If it dies out,
it loses control of the bolus. If it does not, then it is, by definition - a
stationary ring of contracted CM - a sphincter. The point where the p-wave
stops is where we have to look for the sphincter. Yet Ott(11)
probably expresses the consensus of current opinion when he states that the
sphincter ". . . . is not a distinct muscular entity."
Actually, it has been found, accurately described, located and illustrated
as a "muscular ring" in several articles and texts but misidentified as ". .
. . a distinct radiologic and clinical entity." although "relatively rare."
and mostly occurring in children.(12) It is
Wolf's(13) "A ring." It is listed as a cause
of dysphagia for which bougienage and even surgery may be appropriate therapy.(14)
One shudders to think that it may even have been resected!
No one recognizes it as the sphincter(15),(16),(17)
because innumerable manometric reports have conditioned even radiologists to
be looking for a 3 to 5 cm constriction below the diaphragm, not the actual
9-11 mm sphincter above the diaphragm. Wu states that ". . . . some authors
even dispute their [muscular rings] existence."
The captive bolus phenomenon reveals the sphincter: its location relative to
the mucosal junction (.2-3 cm above), its length (8-11 mm) and its competency.
It becomes apparent at the point where the p-wave stops. There it resists the
considerable back-pressure from the bulb- syringe effect of the Valsalva effort.
When it is forced from below by that pressure, its proximal margin is displayed
in sharp contrast to the relaxed CM of the esophageal body. It then disappears
as the esophagus is dilated by refluxing fluid.
References
Last Updated July 26, 2007 by David PJ Stiennon
1. 1. Johnson, Lawrence F., Overview: physiology of the lower esophageal sphincter. In: Esophageal Disorders, Eds. DeMeester, Tom R. and Skinner, David B., Raven Press, New York, 1985.
2. 2.Lerche, W., The esophagus and pharynx in action. Charles C. Thomas, Springfield, Illinois, 1950.
3. 3.Wolf, B.S., The inferior esophageal sphincter - roentgenologic and manometric correlation, contradictions and terminology. AJR 110: 260-77, 1970.
4. 4. Ott, David J., Gelfand, David W., Wu, Wallace C., et al., Esophagogastric region and its rings. AJR :142, 281-7, 1984.
5. 5. Clark, John, A critical look at reproducibility of distal esophageal manometry. In: Esophageal Disorders, Eds. DeMeester, Tom R. and Skinner, David B., Raven Press, New York, 1985.
6. 6. Cauthorne, R.T., Vanhoutte, John J., Donner, Martin W. and Hendrix, Thomas R., Study of patients with lower esophageal ring by simultaneous cineradiography and manometry. Gastroenterology 49: 632-40, 1965.
7. 7. Wynans, C.S., Manometric asymetry of the lower esophageal sphincter. Am. J. Dig. Dis. 22:348-52, 1977.
8. 8. Soffer, Edy E, Ambulatory recording of lower esophageal sphincter pressure: adding the missing link. Editorial, Gastroenterology 108:289-91, 1995.
9. 9.Liebermann, D., Allgower, M., Schmid, P., and Blum, A.L., Muscular equivalent of the lower esophageal sphincter. Gastroenterology 76: 31-8, 1979.
10. 10.Liebermann-Meffert, D., Heberer, M. and Allgower, The muscular counterpart of the lower esophageal sphincter. In: Esophageal Disorders, Eds. DeMeester, Tom R. and Skinner, David B., Raven Press, New York, 1985.
11. 11. tt, David J. ,In: Gastrointestinal Radiology, Eds, Gore, Richard M., Levin, Mark S. & Laufer, Igor, Eds., W.B. Saunders, Philadelphia, 1994.
12. 12. u, W.C., Esophageal rings and webs. In Castell, D.O., The Esophagus, Little Brown, Boston, 1992.
13. 13.Wolf, B.S., Roentgen features of the normal and herniated esophagogastric region, Am. J. Dig. Dis. 5:751-69, 1960.
14. 14. Ott, D.J., Gelfand, D.W., Wu, W.C. and Castell, D.O., Esophagogastric region and its rings, AJR 142:281-7, 1984.
15. 15. Ott, David J, Radiology of the oropharynx and esophagus. In Castell, D.O., The Esophagus, Little Brown, Boston, 1992.
16. 16. Goyal, R.K., Clancey, J.J. and Spiro, H.M., Lower esophageal ring, NEJM 282:1355-64, 1970.
17. 17.Gastrointestinal Radiology, Gore, Richard M., Levine, Mark S. & Laufer, Igor, Eds., W.B. Saunders, Philadelphia, 1994.