The captive bolus
AND
THE PINCHCOCK AT THE DIAPHRAGM
The "captive bolus" phenomenon(1)
provides the only opportunity to observe swallowing against resistance. A detailed
description of what happens during a sustained Valsalva maneuver allows radiologists
to satisfy to themselves that several reported "diseases" are spurious and that
pouches described as functional components of the lower esophagus are simply
hiatus hernias or a normal response of structures to internal pressures.
From this artist’s reconstruction of the processes detailed in Fig. III.3, A-D, the operation of the pump mechanism can be seen at a glance.
Reprinted from Stiennon, O. Arthur, AJR 99:223-32, 1967 with permission
The test explains why an "empty segment" appears at and above the diaphragm.
It shows that the "diaphragmatic pinchcock" is not due to the diaphragm and
does not play any part in preventing GE reflux. With this traditional underbrush
cleared away, it can be seen that it is the LES and only the LES that prevents
reflux of gastric contents into the esophagus.
The phenomena elicited by the test cannot be explained without the phreno-esophageal
ligament (PEL). The test thus proves the existence and functional role of a
structure that furnishes a key to an understanding of reflux. It clearly shows
the sphincer. It reveals the swallowing act in 3-d.
This is how to do it:
In the prone (right anterior oblique) position, the patient is asked to take
one normal mouthful of barium, immediately after swallowing, take a deep breath,
hold it and make a maximum sustained straining effort, i.e., a Valsalva
maneuver.
In a patient with a "positive" test, the barium column is pinched off at and
for a variable distance above the diaphragm. This constriction is the so-called
"diaphragmatic pinchcock." A peristaltic wave then forms in the proximal esophagus
and advances at a uniform rate of about 4 cm/second forcing barium ahead of
it until it reaches the physiologic sphincter. Peristalsis continues to the
lower margin of the sphincter and stops. The sphincter remains contracted either
briefly or as long as the patient can hold his breath. Trapped between the sphincter
above and the "pinchcock" below is a bolus of barium. This is the captive bolus.
Experience shows that the success rate of this demonstration depends largely on the clarity, redundancy and enthusiasm with which one gives the instructions. Getting it right the first time seems important. If the patient starts straining too late and the procedure is repeated, the findings are seldom as clear-cut.
The mechanics of the captive bolus
This is what is happening: When the patient takes a deep breath the phrenoesophageal ligament (PEL) is stretched between its attachment to the diaphragm and the distal esophagus. The PEL forms a "skirt" or tent attached to the esophagus at its apex and with its lower edge flaring out to its attachment on the inferior surface of the hiatal circumference.
As the intrathoracic pressure builds with straining against a closed glottis,
the fundus, drawn into the hiatus by its attachment to the esophagus, is collapsed:
a.) laterally by intrathoracic pressure and b.) from below by (incompressible)
abdominal tissues crowded into the base of the PEL tent by increased abdominal
pressure. Because thoracic air is compressible and the tissues in the tent are
not, the pressure from below wins, the tent becomes convex or dome shaped and
the portion of the fundus within the tent is occluded.
This occlusion sets up the distal barrier that arrests the bolus when it arrives.
Note that 1.) If the PEL is not stretched enough to form a tent, this barrier
cannot be set up. 2.) If the PEL does not exist, the barrier cannot be formed.
Thus we have a means of testing whether the PEL is intact but stretched or ruptured.
The obstruction at the diaphragm is not obvious until peristalsis begins distending
the distal esophagus. One reason for telling the patient not to take a very
large mouthful is that if the bolus is too large the circular muscle cannot
bring the esophageal walls into contact and peristalsis aborts.
Assuming this is not true, a peristaltic wave will form in the cervical esophagus
and push the fluid barium ahead of it. As it moves down the esophagus the lumen
distends because the same amount of fluid is now contained in a shorter tube.
Distention of the lumen (and circular muscle) is the stimulus to LMC,(2)
so, as the peristaltic wave moves distally, the circular muscle ahead of it
is progressively distended and the LM progressively contracted. A maximal distention
produces a maximal LM contraction that pulls the gastric pouch farther through
the hiatus.
During the test, the fundus of the stomach rises above the diaphragm synchronously
with the advance of the p-wave. Despite the transtraction of the stomach through
the hiatus, no esophageal redundancy appears because LM is shortening it.
Although, judging from manometric tracings, one might think the p-wave was
simply an advancing ring of CM contraction, in reality it is a complex advancing
cone of CM contraction. Initially, the cone is long and gradually tapering.
As it progresses distally, it becomes shorter so that by the time it reaches
the sphincter it has shortened to a ring. While the region of CM actively contracting
is 8-10 cm or more, a corresponding region of LM can be presumed activated.
At this point there are two almost turnip shaped "pouches" base to base. The
ancients thought these were some kind of sphincter mechanism. Distinguished
anatomists' names became attached to them furthering the impression that they
were anatomical structures with specialized functions. It is now generally accepted,
however, that the lower pouch is gastric fundus and not a "fore-stomach." The
upper, of course, is the "phrenic ampulla." Unlike the "vormagen," the phrenic
ampulla is always considered a separate anatomical element of the esophagus
and, as such, teleological thinking presumes it should have a distinct function,
presumably sphincteric.

(A) The patient is swallowing barium in the normal fashion. The sphincter (a) is situated 1 to 2 cm. above the diaphragm (b). The phrenoesophageal ligament (c) is slack (B) When the patient strains, the longitudinal muscle of the esophagus contracts, the phrenoesophageal ligament is retracted above the diaphragm and forms a tent-like enclosure. The esophageal mucosa becomes redundant and forms a web or ring (d). Intra-abdominal pressure forces loosely attached structures near the hiatus (e) into the tent of the phrenoesophageal ligament, distending it and at the same time compressing the “herniated” segment of the stomach (f). Meanwhile a peristaltic wave has formed, progressing as far as is possible distally in the esophagus and terminating at the lower margin of the physiologic sphincter which remains closed. The barium trapped between the pinchcock at the diaphram and the physiologic sphincter is the “captive bolus.” The zone (g) below the lower margin of the physioloic sphincter and above the web represents a region having unique physiologic properties. See text. (C) As the maximal straining effort of the Valsalva maneuver is sustained, the physiologic sphincter is unable to withstand the hydrostatic pressure generated by further encroachment of the abdominal structure into the phrenoesophageal tent. This results in proximal ejection of a jet (h) from the captured bolus. Reprinted from Stiennon, O. Arthur, AJR 99:223-32 19 with permission
When the p-wave reaches this point, all activity stops. The obstruction persists, the p-wave has reached the end of its travel and the bolus is trapped between the two. That this condition may persist since the patient can maintain the Valsalva effort tells us something. The now ring-like p-wave, without any auxiliary support, is entirely capable of containing the bolus against the considerable hydraulic pressure of the tissues being forced into the tent of PER like a thumb on a bulb syringe. It has become the sphincter. By now high above the diaphragm, there are no other sphincter candidates in the region.
Lessons of the captive bolus test
These simple mechanics also explain a great deal about the GE junction, sphincters
and hiatal hernias. First, it explains why there is sometimes a pinchcock-like
mechanism at the diaphragm and why it is sometimes lacking: The subdiaphragmatic
soft tissues crowding into the tent-like PEL collapse the tube of gastric fundus
drawn into the tent by contraction of the LM. The barium column, therefore,
appears "pinched" or occluded.
Some have supposed that it was the diaphragm itself that caused this constriction.
However, the pinch effect is not limited to the level of the diaphragm - the
diaphragm is only a few millimeters thick - but extends both above and below
the diaphragm.
As Hayward has emphasized, the PEL is an exceedingly elastic structure ".
. . rich in elastic fibers" that " . . . if divided near the esophagus . . .
may be taken right up into the adventitia of the esophagus and vanish." If the
PEL is not stretched or elongated, no tent will erect and there is no pinchcock.
Therefore, a CB is itself a sign of hiatus hernia (HH) because that is what
a sliding HH is - a stretched, elongated PEL. The reason it is a sliding
HH, is that an intact, elastic PEL provides the reducing force. LMC stretches
the PEL and pulls a tube or pouch of fundus above the hiatus; the elastic recoil
of the PEL reduces the HH when LMC stops.
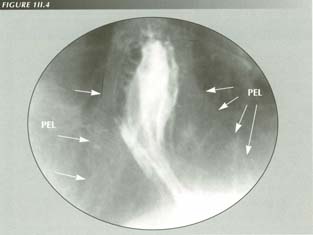
The pinchcock at the diaphragm: the costriction is actually well above the diaphragm and obviously much thicker than the diaphragm. On this lighly exposed film, one can just make out the bell-like tent of the PEL which, by constraining mesentery protruding through the hiatus, chokes off the fundus attached at the apex.
Is the pinchcock a defense against reflux? No. If a patient with a diaphragmatic
pinchcock has a successful HH repair, the pinchcock will disappear. It is illogical,
therefore, to postulate as a normal antireflux mechanism a diaphragmatic pinchcock
that depends on a pathological set of circumstances and that vanishes
when the pathology is removed. This tells us that the pinchcock at the diaphragm
can have nothing to do with the prevention of reflux. It is simply an anatomical
pattern that occurs when the PEL is stretched but not ruptured.
It is generally supposed that a Valsalva test provokes a sliding HH by increasing
intra-abdominal pressure. However, it is not the increased intra-abdominal pressure
per se but the maximal LMC provoked by swallowing against the resistance
of the pinchcock which draws the fundus above the diaphragm.
LMC, by the shortening esophagus, causes mucosal redundancy. As there is a
good deal of elasticity in esophageal mucosa, signs of redundancy do not begin
to appear until the esophagus has shortened 3 to 4 cm. Thereafter, the redundant
mucosa may form a fold or accordion pleat. This is the "Schatzki" ring.
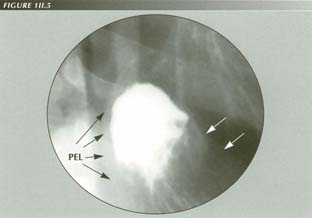
Omentum crowding into the PEL tent. Note the PEL insertion at the sphincter. Although the rest of the PEL is largely invisible, it can be appreciated by the way it constrains the inra diaphragmatic tissues after they protrude through the hiatus.
Why isn't the "ampulla" obliterated by the advance of the peristaltic wave? Because peristalsis stops at the sphincter.
Three results
From these observations, we can establish three results that are neither common knowledge nor consistent with early speculations as to the function of the phrenic ampulla.
The phrenic ampulla does not have any sphincter function
The ampullary dilatation is merely a ballooning of a segment that is incapable of peristalsis.
Most important, however, is this demonstration that the p-wave stops at
the lower edge of the sphincter - which is not necessarily the end of the
esophagus. It is well known that there is normally no peristalsis in the gastric
fundus, but the existence of an aperistaltic esophageal segment, to the best
of my knowledge, has not been observed either radiologically or manometrically.
This fact will assume importance when we consider "achalasia."
The pinchcock may be forced at times, but usually the sphincter is first to
yield so that a retrograde jet of barium squirts up into the relaxed esophagus
proximal to the sphincter. The ease and rapidity (the jet may reach the height
of the aortic arch in .25 seconds) with which the proximal esophagus then fills
demonstrates the lack of tone in the body of the esophagus in the wake of the
p-wave - as we also know from the fall in the manometric pressure tracing behind
the p-wave.
Also illustrated is a unique aspect of LM contraction: unlike CM contraction,
it does not relax in the wake of the p-wave. Instead, the p-wave appears to
latch the LM as it passes through it. Only when the p-wave reaches the sphincter
does the LM relax.

Long PEL:
Although the PEL is difficult or impossible to see in most cases, it produces effects which are unmistakable. Here a Valsalva effort collapses the stomach in the PEL distal to its attachement because hydro-static pressure is confined to the (in this case) tubular PEL tent. This extreme example shows the mechanism responsible for the “empty segment.” It has no part in preventing reflux. Tissues slowly crowding into the PEL have been mistaken for prolapsing mosa
The bulb syringe effect of the PEL tent
The yielding of the sphincter is not due to a further advance of the p-wave,
but to further encroachment on the space within the PE tent by abdominal tissues
crowding into it from below. These act as a piston to create the necessary hydrostatic
pressure to force the bolus back through the sphincter.
If the observer's attention is on the body of the esophagus, he may have the
impression of reverse peristalsis, however, this is not so. Cine-films of this
phenomenon centered on the gastric pouch(4) show
that it collapses in its axial direction before its transverse dimension decreases
appreciably - as though a piston were moving up from below ejecting barium ahead
of it.
When tracings of successive frames of a cine strip of the process are superimposed,
it can be seen that, whereas the outline of upper pouch and sphincter remains
nearly constant, the outline of the gastric pouch moves proximally. Calling
this a piston-like action is scarcely accurate. It is an extremely complex event
with a torus of abdominal soft tissues rolling up into the PEL tent. The net
effect, however, is a piston or bulb syringe-like action.
It is doubtful that this process has any significant role in, say, causing GE reflux. If it occurred during swallowing, no acid would be retrojected. It is also noteworthy that the pinchcock zone is much wider than both the diaphragm and the physiologic sphincter. 1, 2 or 3 prominent gastric folds are usually seen in the constricted area. If only one is seen, the resemblance to the bird beak, described as characteristic of achalasia, is perfect.
Locating the sphincter
The lower esophagus must exhibit either McLean notches or a LER to demonstrate
that the p-wave does not extend to the end of the esophagus but stops at the
lower sphincter margin. About 3 cm is the maximum distance between the ring
and the lower edge of the sphincter I have encountered. Usually this distance
is .5 to 1.5 cm.
One cannot help wondering why the sphincter is not at the very end of the esophagus.
It is a common observation that, except in most unusual circumstances, there
is no peristalsis in the fundus of the stomach. The gastric peristaltic wave
starts high on the greater curvature of the stomach. That the esophageal wave
stops short of the stomach would have been difficult to anticipate. There is
no manometric evidence of an aperistaltic esophageal zone. The aperistaltic
region may act as the opening wedge of the sphincter during belching, vomiting
and reflux when it flares to its trumpet shape.
If the patient is still able to sustain the Valsalva effort, a new peristaltic
wave will form and again force the regurgitated barium into the double compartment
between sphincter and pinchcock. Repeated cycles of this nature may follow without
so much as a drop of barium escaping through the pinchcock.
Antireflux significance
If one studies the captive bolus during its arrested phase, it is easy to see that:
There is no angle of His in sight.
The right crus of the diaphragm is well below the area of interest.
There is no subphrenic esophagus.
The area of muscular thickening at the GE junction described by Liebermann-Meffert
et al.(5),(6)
is 9-21 mm below the squamo-columnar junction - which, as we know,
is exactly at the LER. This would place the thickening in the upper portion
of the "herniated" (actually retracted) fundus where it clearly is not playing
any part in the obstructing mechanism or even influencing the shape of the fundus.
The sling fibers of the stomach are also completely overpowered by other forces and nowhere in evidence.
Yet, despite the absence of any of the classical configurations invoked as antireflux mechanisms, the unaided sphincter is doing a magnificent job of remaining competent. Even the considerable pressure built up by upper abdominal tissues crowding piston-like into the confining tent of PEL does not force it.
The illusion of prolapse
Turning attention again to the incursion of a torus of abdominal soft tissues
into the base of the PEL tent, we can see that as this occurs, mucosal folds
appear to be moving proximally into the gastric pouch, but this is simply because
its walls are coming into contact. If only the retrograde mucosal margin is
noted, it will be mistaken for "retrograde prolapse of gastric mucosa"(7),(8),(9)
into the esophagus unless morphological details are carefully analyzed.
Of course, all of this is happening in a relatively few seconds and, without
the aid of cinefluoroscopy or a sequence camera, analysis of the process is
difficult. Prolapse of esophageal mucosa into the fundus has been reported(10),(11)
repeatedly, but it is very unlikely that this occurs. If it did, there would
be no reason for a ring to form. For some reason, the enteric mucosa, that is
so loosely attached to the wall in the esophagus, is firmly attached in the
fundus. Instead, the motion of the torus into the tent simulates sliding or
prolapsing mucosa - gastric when it is rising and esophageal when it is reducing.
Strange formations are seen at the end of the CB test when the pouch of fundus
above the diaphragm begins to return to its normal infradiaphragmatic position.
As mentioned, the PEL provides the restoring force. It is applied at the apex,
rather than the base of the retracted pouch of fundus. Therefore the soft tissues
- both the fundic pouch and supporting omentum, etc. - are pushed into
the abdomen. Like a crowd of people escaping a theater fire, these tissues tend
to overrun the exit. The result is the interesting shapes aptly described as
"arum lily," "Jack-in-the-Pulpit," "Saturn ring" or "wing sign" as the fundic
pouch telescopes into itself or overhangs the diaphragm. These signs do not
suggest any special disease states.
Finally, we are able to explain why a Valsalva maneuver demonstrates sliding hiatus hernias. It does so by occluding the alimentary tube thus provoking maximal peristalsis and maximal LM contraction. With normal swallowing in the upright position, LMC is minimal. With swallowing against an obstruction, however, peristalsis becomes more forcible and LM contraction acts to pull the esophagogastric tube, stocking fashion, over the bolus pulling the gastric fundus into the chest in the process. In a subsequent chapter a more extensive proof of the cause of hiatus hernias will be elaborated.
SUMMARY
A detailed study of the minutiae of the captive bolus phenomenon yields results that we can use in the proof of many propositions throughout this presentation. Among them the following:
The LM shortens as peristalsis proceeds down the esophagus.
There is an aperistaltic segment that corresponds to the phrenic ampulla and
accounts for its formation.
The elasticity of the phrenoesophageal ligament is the restoring force in
sliding HH. The size of the sliding HH is a measure of the stretch of which
the PEL is capable.
The 2-pouch appearance is explained.
The "Saturn ring," "arum lily" and "wing signs" are stages in the reduction
of a sliding HH.
Retrograde prolapse of gastric mucosa and orthograde prolapse of esophageal
mucosa are misinterpretations.
The pinchcock at the diaphragm is not due to the diaphragm, is not a part
of the anti-reflux mechanism and could actually cause reflux.
The physiologic sphincter is less than a third the length it is judged to
be manometrically.
The LES is not only highly competent in the face of extreme retrograde pressure, but is the sole anti-reflux protection of the esophagus. It is present and functioning when there is no evidence of an angle of His, subphrenic esophageal segment, pouting of the gastric or esophageal mucosa, valve of Guberoff, etc. In the next chapter I will discuss some more fundamental misconceptions about the sphincter.
References
Last Updated July 26, 2007 by David PJ Stiennon
1. 1. Stiennon, O. Arthur, The "Captive Bolus" test and the pinchcock at the diaphragm: an esophageal pump and some non-diseases of the esophagus. Am. J. Roentgenol. Tad. Therapy and Nuclear Med. 99:223-32, 1967.
2. 2. Christensen, James and Lund, Gordon, Esophageal response to distention and electrical stimulation. J. Clin. Invest. 48:408-19, 1969.
3. 3. McLean, C.D.T., Lower esophageal ring or groove. Brit. J. Radiol. 31:472-6, 1958.
4. 4. Stiennon, O. Arthur, 1967, op cit.
5. . Liebermann-Meffert, D., Heberer, M. and Allgower, The muscular counterpart of the lower esophageal sphincter. In: Esophageal Disorders, Eds. DeMeester, Tom R. and Skinner, David B., Raven Press, New York, 1985.
6. . Liebermann, D., Allgower, M., Schmid, P., and Blum, A.L., Muscular equivalent of the lower esophageal sphincter. Gastroenterology 76:31-8, 1979.
7. . Fagan, C.J. and Palmer, E.D., Gastroesophageal retrograde prolapse. Am J. Roentgenol., Rad. Therapy & Nuclear Med. 90:774-7, 1963.
8. . Feldman, M., Retrograde extrusion or prolapse of gastric mucosa into the esophagus. AM. J. Med. Sci. 222:54-60, 1952.
9. . Kerr, Robert M. Hiatal hernia and mucosal prolapse. In: The Esophagus, Ed. Castell, Donald O., Little, Brown and Company, Boston, 1992.
10. . Aldridge, N.H., Transmigration of the lower esophageal mucosa. Radiology 79:692-68, 1962.
11. . Russell, W.J. and Kogure, T., Transmigration or prolapse of esophageal mucosa. Am. J. Roentgenol. Rad. Therapy & Nuclear Med. 92:1017-20, 1964.