"Hiatus hernia" and rupture of the PE ligament
Like "achalasia," "hiatus hernia" is an example of a wrong name paralyzing
thinking about a disorder. Because they are called hernias, "hiatal hernias"
are lumped in with inguinal, femoral and ventral hernias. We tend to assume
that our instructors gave us the correct names for things! Standard
references(1)(2)(3)(4)(5)(6)
do not even discuss their pathogenesis. It is simply taken for granted. After
reviewing 636 references, Postlethwait(7) concludes
they are due to increased intra-abdominal pressure in combination with weakness
of the supporting structures.(8) Even a group(9)
that reported experimental production of hiatus hernia by vagal stimulation
concluded that most were due to increased intra-abdominal pressure. A recent
review(10) lists 17 possible causes, except
for increased intra-abdominal pressure, most of them nonspecific.
The central problem of "hiatus hernias" (HH), therefore, is to prove that they are not hernias. Instead, I must show that the condition is a traction phenomenon - that the fundus is drawn above the diaphragm by the tractive force of longitudinal muscle contraction (LMC).
Support for this position is many-sided:
The function and power of the longitudinal muscle are appropriate to the task.
Vagal stimulation of the longitudinal muscle will produce hiatal "herniation."
The morphology of the various types of HH is inconsistent with their supposed
origin by pressure from below the diaphragm; it is exactly consistent with a
traction mechanism.
The frequency distribution (90% sliders -- 10% others) is only consistent
with a traction pathogenesis.
Extrinsic traction, such as that produced by cervical hyperextention (whiplash
injuries, Sandifer's syndrome), also causes HHs.
The near 100% association of Zenker's diverticulum with HH is a further line
of proof for a traction mechanism.
Because ideas are embedded in words, it is appropriate to start with a definition:
A hernia is "a protrusion of an organ or part . . . through the wall of a cavity
in which it is normally inclosed."(11) Further
protrude is defined "L, protrudarei, to thrust forward, to
cause to project or stick out." and, finally, "project, to throw out."
Again, Dorland(12) attributes to Celsus the
definition: "The protrusion of a loop or knuckle of an organ or tissue through
an abnormal opening." [Emphasis added.]
The fundamental idea here is that the force that causes the "throwing" and
"causing to project or stick out" is behind the thing thrown. The gunpowder
is behind the projectile. The rocket thrust is from behind.
And so it is with most hernias. The force that causes the organ to "protrude
or stick out" is behind the organ and inside the space from which it is protruding.
This is an entirely correct concept whether we are speaking of an inguinal,
a ventral or an umbilical hernia; whether we are describing a mediastinal hernia,
an intercostal hernia, a herniation of the cerebellum or of the nucleus pulposus
of an intervertebral disk. It may even be true of protrusions through the diaphragm
at the foramina of Bochdalek and Morgagni. The same mechanism (increased intra-abdominal
pressure) is assumed to be etiologic for "hiatus hernias," but is not. (I
will call them "HHs" from now on to avoid the awkward but necessary quotes.)
This unfortunate choice of a name and our innate feeling for the meaning of words has virtually closed the door to an understanding of the cause, effects and treatment of HH. The semantic disability is difficult to cure because there does not exist, in English at any rate, a word meaning "External traction on an organ or part pulling it out of the cavity that normally contains it." Perhaps this is not surprising; there would be only two situations to which it could apply.(13)
HHs differ from abdominal hernias
HHs do not fit the definition of hernia and are not analogous with hernias.
Hernias occur through an abnormal weak spot in the wall of a body
cavity. HHs occur through a preformed, normal opening.
In HH, the protruding organ is a continuation of an organ, the esophagus,
in another body cavity. No true hernia is so constituted.
Unlike abdominal hernias, transients aside, the basic hydrostatic pressure
differential across the wall of the containing body cavity that favors protrusion
is lacking in HH.
No true hernia is ever drawn from its proper body cavity by traction from
without. HHs are.
True hernias can be repaired by reinforcing or occluding the weak area in
the wall of a body cavity. Without severing the esophagus, the esophageal hiatus
cannot be closed.
Laboratory studies
As early as 1932, Von Bergman and Goldner(14)
had suggested that HH might be due to traction due to esophageal shortening
in response to vagal stimulation. They quoted earlier experiments of Kuckuck
showing that stimulation of the vagal trunk produced hiatal herniation in rabbits.
Sir Arthur Hurst, of achalasia fame, subscribed to a similar hypothesis.(15)
In 1945 Dey, Gilbert, Trump, Roskelly and Rall(16)(17)
experimentally produced HHs in dogs by stimulating the proximal end of the transected
vagus nerve, by stimulating the intact vagus and by peritoneal or upper abdominal
organ stimulation. Later (1967) Torrance(18)
found an identical response in cats and may have been the first to associate
both HH and reflux with LMC.
In 1969 Christensen and Lund(19) performed
much the same experiment on the opossum (Didelphis virginiana) as this
animal has the same distribution of striated and smooth muscle as is present
in humans and, conveniently, has a 4-cm intra-abdominal esophageal segment.
It enters the stomach just proximal to the pylorus instead of inserting in the
fundus. They found that stimulation of the esophagus in vivo by distending
an intraluminal balloon produced ". . . visible shortening of the intra abdominal
segment with rostral sliding of the esophagus into the diaphragmatic hiatus."
A GEDANKEN EXPERIMENT
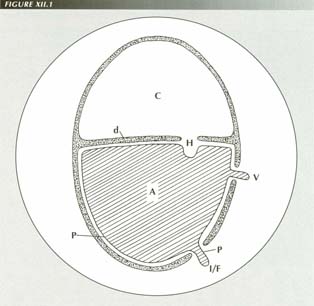
The oval represents the muscular wall of the thorax and abdomen lined, in the case of the latter, with peritoneum. In the static acase, the abdominal contents act as a “bag of water” and, with normal abdominal tone, will tend to extrude the peritoneum through gaps in the wall, forming ventral hernias at “v” and inguinal and femoral hernias at “I/F” by hydrostatic pressure. There is no hydrostatic pressure on the top of the bag of water. If anything, a membrane closing the hiatal gap “H” would sag downward. If the muscualr wall contracts, the abdominal pressure increases and the hernias are exaggerated. However, any pressure gradient at the hiatus is equalized by upward or downward dispalcement of the diaphragm.
Transducers connected to the distal esophagus of the cat, opossum and monkey
by Dodds, et al.(20)(21)
demonstrated that ". . . a forceful longitudinal tug is generated during esophageal
peristalsis." These authors also suggested LMC as a possible factor in the genesis
of HH. Daintree Johnson(22) (1966) produced
hiatal transtraction in dogs by stimulating LMC with apomorphine.
As these studies have not made much of an impression or perhaps are regarded as tentative or as laboratory curiosities, I will consider at length and from every conceivable angle the etiology of this common disorder. I wish to show that LMC causes not just the occasional HH, but all of them.
A radiological misconception
The usual method of eliciting abdominal hernias is with the Valsalva maneuver
- forced expiration against a closed glottis, but this also elicits HHs and,
perhaps because of this, HHs are presumed to be etiologically identical with
other hernias. Despite the superficial resemblance, however, there is a fundamental
difference. A Valsalva maneuver elicits a sliding HH only when a bolus
is being swallowed during the maneuver. The distention of a bolus causes enough
LMC to erect the PEL tent, after which increased intrathoracic and intra-abdominal
pressure occlude the lumen of the portion of the fundus in the tented PEL. Thereafter,
swallowing must occur against resistance. The near-maximal LMC provokes the
HH via the captive bolus effect.(23)
Thus, although straining against a closed glottis also produces HH, it does
so not because it increases intra-abdominal pressure relative to the
thorax, but because it provokes LMC. It is easy to see why an observer
could have the impression that the gastric segment is being extruded upward.
If this were the case, however, the esophagus would become redundant and either
telescope into the fundus or be pushed aside by the extruding stomach (as does
happen with non-sliding hernias). Instead, the esophagus is short and taut as
a bowstring.
A gedanken experiment
To refute the increased intra-abdominal pressure pathogenesis, it is useful
to perform a "gedanken experiment" such as those used by physicists in thinking
about situations it would be difficult or impossible to set up practically.
As, hydrostatically, the abdomen behaves like a bag of water,(24)
we start by imagining a muscular cylinder divided into two compartments by a
flexible, diaphragm-like partition. The lower compartment is lined by a thin
elastic membrane (peritoneum) and is filled with water. The upper compartment
is filled with air at normal atmospheric pressure.
If holes or weak spots are then created in the cylinder wall, the elastic
membrane, driven by the force of hydrostatic pressure, will bulge through the
holes in typical hernia fashion. Those that are lowermost will bulge the most
because there is a greater head of hydrostatic pressure extruding them.
Next, without perforating the lining membrane on its inferior surface, we
make holes in the "diaphragm." How much will the membrane bulge through these
holes? Not at all. There is zero hydrostatic pressure at the top of the fluid
filled cavity. In fact, if the "diaphragm" were inflexible, the lining membrane
would bulge downward, because the volume would remain constant and
any extrusion below would be matched by intrusions of equal volume on top.
We conclude that, given the constant hydrostatic pressure relationships, ventral
and inguinal hernias will occur simply from hydrostatic pressure on a locus
minoris resistentia, but diaphragmatic hernias would never occur. Indeed,
the very opposite would be the case.
Of course, it is possible to increase intra-abdominal pressure by performing
a Valsalva maneuver. In the gedanken experiment, this would be simulated by
a contraction of the entire muscular cylinder. It is apparent that a manometer
connected to the fluid-filled chamber would register an increase. The membrane
would bulge farther out of the "hernias."
Would there now be an upward bulge through the holes in the diaphragm? No,
because the air pressure above the diaphragm is now increased by an amount that
is exactly equal to the elevation caused by the muscular contraction in the
lower compartment. The pressure gradient across the diaphragm remains unchanged.
In the experiment, as in the body, it is impossible to contract only the wall
about the air chamber or only about the water chamber. Any transient differential
is immediately compensated by an upward or downward motion of the diaphragm.
The only way an upward protrusion through the holes in the diaphragm could occur
- in man or in the experiment - is if the diaphragm could move downward without
expanding the abdomen.
These pressure relationships are, of course complicated by transient effects,
blows to the abdomen, etc. However, they explain why hernias seldom occur at
the other superior openings in the diaphragm, e.g., those for the aorta and
inferior vena cava or the foramina of Bochdalek and Morgagni or via the transdiaphragmatic
lymphatics or at the fat-filled openings in the diaphragm seen on 6% of CT examinations.
An eventrated diaphragm may be so thin as to be little more than its membranous
investments, yet organs do not herniate through it. Such a thinning of the abdominal
wall would lead to gross herniation.

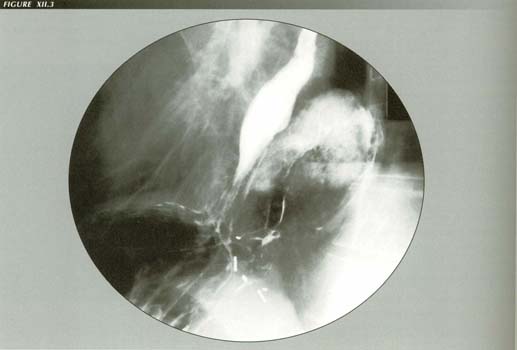
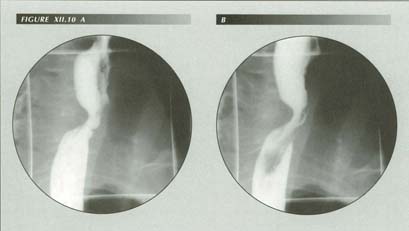
Ruptured PEL: A slight molar tooth shape results when the esophagus invaginates the stomch. Note the poor effacement of the LES.
The explanation, of course, is the special circumstance that a powerful muscle is pulling the stomach through from above. The force of a LM contracting up to 42% of its resting length is what does it.
HH morphology is only consistent with LMC pathogenesis
A further line of proof that traction from LMC causes HH is more extended.
It is of considerable radiological interest, however, because it explains the
morphology of the several types of HH. The argument is based on the classification
and relative frequency of the three classical types of HH. It also explains
the relative frequency of each and leads to an understanding of the role of
the PEL in HH.
Following Akerlund(25) we can define three
types:(26)
Type I - The Axial or sliding HH
Iatrogenic hiatus hernia: This is the sole example of a “paraesophageal HH” I have been able to collect. Although, it is iatrogenic, this is the way one should look. The esophagus is attached to the diaphragm and the stomach protrudes alongside it. If HHs were due to chronic or intermittent increases in intraabdominal pressure, this should be the most common variety of all.
Type II - The "molar tooth" variety
The "tooth" appearance is due to the distal end of the esophagus telescoping
into the fundus of the stomach. It occurs in older patients and its demonstration
does not require a Valsalva test. It can be elicited by using a bolster, pressure
on the abdomen, bending forward or - most commonly - without any maneuver at
all. Gas in the stomach, or merely the buoyancy of the attached omentum, floats
the fundus through the hiatus into the chest. It is larger than the type I hernia.
It either has a molar tooth shape or a pronounced angle of His is present, but
not both. The captive bolus test is negative. It tends to be asymptomatic.
Type III - The "paraesophageal" variety
Although the distinction is seldom made,(27)
the name "paraesophageal hiatus hernia" can be understood in 2 ways: a.) as
meaning a hernia through the esophageal hiatus alongside of the esophagus
or b.) as a hernia through the diaphragm beside the esophageal
hiatus. The distinction may be moot as both are so rare their very existence
is questionable. The published illustrations appear to be large Type II HHs.
Both the fundus and the gastroesophageal junction are above the diaphragm.
For either definition to apply, the GE junction would have to be normally situated
at the diaphragm.
In these large hernias, the fundus, instead of telescoping over the shortened
esophagus, can float up into the chest beside the esophagus in a way that produces
an acute "angle of His." This has been a source of confusion. A paraesophageal
HH would have a sharp angle of His because, while the esophagus remained securely
anchored by the PEL, the fundus of the stomach, having broken through the PEL,
would lie in contact with its lateral aspect.
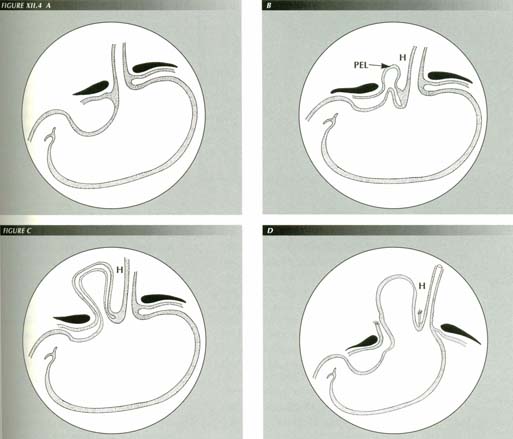
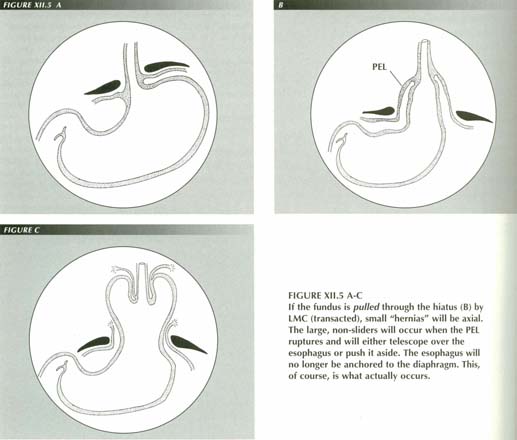
FIGURE XII.4 A-D
If hiatal “hernias” were due to pressure from below, small “hernias” would be paraesophageal. The progression would be from A to B as the weakest area of the obturating PEL yielded to pressure. As the weak spot stretched (C), a hernial sac would form next to the esophagus. The latter would still be firmly anchored to the diaphragm by the unimpaired portions of the PEL. Finally, (D) the PEL would rupture locally and the adjacent stomach would extrude through the gap. But early, small HHs are never paraesophageal as this mechanism would predict.
H = Angle of His
The morphological feature that makes a HH truly "paraesophageal" is a firm attachment of the esophagus to the diaphragm to the right of the fundus. The appearance may be simulated by the slope of the diaphragm, but one can always prove unequivocally that the HH is not paraesophageal if the lesser curvature of the stomach in indented by the diaphragm in any projection as this could not occur if the PEL were still intact.
TABLE 1
Comparison of Type I and Type II hiatus hernias
| Radiologic sign | Slider | Non-slider | |
| 1 | Size | up to 8 cm | larger than 8 cm |
| 2 | Self-reducing | yes | no |
| 3 | Captive bolus test | positive | negative |
| 4 | Axial | yes | variable |
| 5 | Diaphragmatic notch | no | yes |
| 6 | Reflux | frequent | seldom |
| 7 | Angle of His | never | frequent |
| 8 | Esophagus | taunt | redundant |
| 9 | Associated LER | frequent | seldom |
| 10 | Shape | bell, turnip | molar tooth |
| 11 | Frequency | 90% | 10% |
| 12 | Age | younger | older |
| 13 | Sphincter effacement | complete | incomplete |
This diversity of morphology (Table 1) has a unifying principle: the PEL
is intact in Type I (sliders) and ruptured in the other(s). Although the
PEL is a structure that can be visualized directly only in part, its presence
is manifested by the way it affects the fundus and esophagus.
1. Size: The slider remains small - the vast majority of them
are 4.5 cm in length and they rarely exceed 7-8 cm -- because the esophagus
is tethered to the diaphragm by an intact PEL. Once the PEL ruptures, nearly
the entire stomach can rise above the diaphragm because its only restraint is
then the gastric attachment to the retroperitoneal portion of the duodenum.
2. Self-reducing: When the LM contracts, it stretches the
PEL. The sliding HH reduces spontaneously because there is a restoring force
- the elasticity of the PEL. Once the PEL ruptures, there is nothing to pull
the fundus back into the abdomen when the LM relaxes. Reduction of sliders is
sometimes partial as, to the extent the PEL is permanently elongated, it cannot
completely reduce the HH.
3. Captive bolus: The captive bolus phenomenon depends on
an intact PEL to constrain abdominal tissues about the fundus and so obstruct
it. Thus, it is positive in sliders and fails when the PEL ruptures. Although
the Valsalva maneuver may also provoke a Type II HH, it is not necessary as
even a gas bubble in the fundus can float it through the hiatus once the PEL
is gone.
4. Axial: The slider is axial because it is retracted from
above by the LM. The Type II HH is not axial because, once the PEL ruptures,
the fundus follow the path of least resistance, either rolling by ("periesophageal")
or telescoping over ("molar tooth") the esophagus. Because the LM is no longer
involved in HH production at this stage, the esophagus does not contract and
get out of the way of the herniating fundus.
5. Diaphragmatic notch: Once the constraining effect of the
PEL is destroyed, the stomach can slide freely through the hiatus. The diaphragm
forming the left edge of the hiatus then causes a distinctive notch on the greater
curvature that moves up and down the curvature with respiration as the stomach
remains stationary while the diaphragm moves.
6. Reflux symptoms: Oddly enough, patients with the larger
Type II HHs picked up on admission chest films the patient may be asymptomatic.
Earlam,(28) for example, states, ". . . they
are not associated with gastroesophageal reflux." Paradoxically, the symptoms
are inversely related to size. This tells us that an intact PEL is a factor
in reflux. This connection will be discussed in detail in the chapter on gastroesophageal
reflux.
7. Angle of His: The angle of His is only a potential angle.
Normally, esophageal LM tone keeps the fundus snugly against the under surface
of the diaphragm obliterating the angle. Once the PEL ruptures, the angle can
form because the entire fundus is above the diaphragm
8. Taunt esophagus: Because it provides the motive force,
the LM is taunt when retracting a slider but (usually) passive and relaxed during
the occurrence of a Type II HH. This may seem a subtle distinction, but fluoroscopically
it is a reliable distinguishing sign.
9. Associated LER: These are more common with sliders because
the esophageal mucosa never has an opportunity to adapt to a shortened state.
When the esophagus relaxes, the elastic PEL restores its length. Just as a sphincter
can close but not open itself, a longitudinal muscle can shorten but not elongate
itself. Once rupture destroys the length-restoring force of the PEL, the esophageal
mucosa can fit to a shortened organ and so lose the redundancy that is necessary
to form the accordion-pleat fold. A LER may then disappear, become less prominent
or become shallower and thicker.
10. Shape: Only when the PEL is ruptured can the stomach telescope
over the end of the esophagus or roll alongside of it.
11. Frequency: Sliders outnumber other types about 10 to 1(29)
because they represent the initial stage of a process. Not every stretched PEL
goes on to rupture. However, the tendency is to an increase in size with the
passage of time. Of 19 patients followed 6 or more years by Sprafka et al.,(30)
11 (58%) showed progression from small to large HHs
12. Age: The longer the PEL is exposed to the trauma of swallowing
many thousands of times daily, sustained hypertonia of the LM, belching, gagging
or episodes of vomiting, the more likely it is to rupture. Hence the older age
of the patient with the ruptured PEL.
13. Sphincter effacement: A frequent finding in PEL rupture
is a thicker ring like narrowing at exactly the location of the physiologic
sphincter (1-2 cm above the ora serrata). It is about 1 cm in length instead
of web-like. It represents the uneffaced physiological sphincter itself - uneffaced
because an essential element of the effacement mechanism, the PEL, has been
destroyed.
Basically then, the PEL is what determines the morphology of the GE junction. Although this conclusion was reached by a phenomenological route, it is possible to demonstrate the actual ragged skirt of ruptured membrane radiographically in Type II HHs if one searches for it.
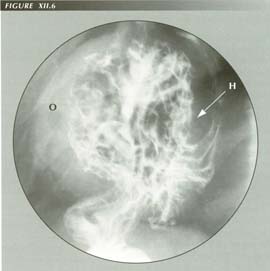
Rupture of the PEL and the angle of His: Because of the acute angle of His, it has been assumed that this condition is a paraesophageal hernia. However, it is obvious that the esophagus is not attached to the diaphragm at any point due to complete rupture of the PEL. The stoamch floats into the chest either alongside the shortened esophagus, producing the acute angle of His seen here, or else telescopes over it to produce the “molar tooth” appearance. Once the PEL ruptures, the patient’s reflux may be cured! This is responsible for the belief that the angle of His prevents reflux. Note the fatty mesentery along the greater curvature.
H = Angle of His
O = Omentum
One should, perhaps, be diffident in refuting the opinions of surgeons who
have had the benefit of exploring these patients and yet have reported many
"paraesophageal" hernias. Surely, they would note whether or not the PEL was
intact on one side of the hiatus. Evidently, however, they just accept the radiologist's
classification without making a point of examining this critical connection.
In type II HHs one can see a sliding constriction in the stomach as it passes
through the diaphragm. It slides down the stomach on inspiration and up on expiration.
In doing so it rubs the longitudinal rugae against each other promoting erosions
and bleeding -- the so-called "watermelon stomach."(31)
I do not wish to give the impression that the differential diagnosis between
the two types of HH is always sharply etched. There are stretched, inelastic
PELs that can confuse the issue by presenting some signs of each variety. Nevertheless,
usually, the differential is obvious.
As an alternative name for Type II and III HHs, "rupture of the PEL" is somewhat
of a simplification. There are 5 layers of tissue in the PEL and any combination
of them can lose its elasticity allowing the others, e.g., the pleura or peritoneum,
to stretch and so conceal the rupture of the elastic connective tissue that
forms the ligament proper.
The genesis of HH
It is the absence of paraesophageal HHs that makes a compelling contribution
to the proof that LMC causes HHs. Although it has been shown that the steady
state hydrostatic pressure at the diaphragm is zero, what about transients -
cough, sneeze, blows to the abdomen, etc.? The skirt of PEL obturates the hiatus.
If transient elevation of intra-abdominal pressure were the cause, a herniation,
if it occurred at all, would first work its way through the weakest part
of the PEL. As the entire circumference of the PEL would hardly weaken simultaneously
to the same extent, most early, small herniations would be paraesophageal extrusions!
This is exactly the reverse of what actually occurs.
Traction from above, on the other hand, stretches the entire PEL without initially
rupturing any of it. We know that Type I sliders far outnumber all the rest.
The obvious conclusion is that the smaller, sliding HH is an earlier stage of
the larger, Type II HH. Rupture of the PEL is the event that converts a Type
I to a Type II.
The morphology and frequency distribution of the various types of HH, therefore,
are consistent with traction from above and inconsistent with the conventional
assumption they are caused by pressure from below.

RUPTURE OF THE PHRENOESOPHAGEAL LIGAMENT:
The very elastic PEL provides both the inferior attachment of the esophagus and the force that restores the esophagus to its normal resting length and reduces the sliding HH. In a huge HH such as this, the esophagus is permanently shortened because the elastic PEL is ruptured. Consequently these HHs do not “slide.” Resolution of the force of LMC by the PEL also creates the sphincter-opening vectors. When the PEL ruptures, this mechanism is destroyed and the sphincter does not efface well although a bolus will usually distend it. this non-effacement is a not uncommon cause of dysphagia. By the same token, the LMC and hiccups can no longer open the sphincter. These patients usually experience symptomatic remission! This is the explanation for the paradox that the largest HHs are the least symptomatic. Note that the true length of the LES (8 mm corrected for magnification) is much lesss than it is judged to be by manometric methods. Although one can infer that gastric mesentery herniates along the the fundus in HH, this illustration shows it directly (arrows) proving that it extends to the GE junction. Without the restroring elasticity of the PEL, the esophagus does not alternate betweeen short and long. The mucosa no longer needs an accordion pleat, therefore, and LERs are seldom seen after rupture of the PEL.
The analogy with the ureter
The esophagus and the ureter are comparable organs. Their walls are composed
of alternating layers of circular and longitudinal muscle. They are both fixed
at either end instead of being loosely coiled like the intestine.
Physiologically both organs have one-way characteristics as there is a physiologic
need to prevent reflux from the stomach in the one case and the bladder in the
other. The esophagus cannot easily tolerate acid and the kidney cannot tolerate
ascending infection from the bladder.
Pathologically, the main diseases of both organs result from failure of their
one-way characteristic with reflux from the terminating organ. A large literature
has grown out of the resulting problem of vesico-ureteral reflux and its treatment.
I shall not attempt to analyze or digest it but merely point out that the analogy
with the esophagus is not a superficial one.
Just as the esophagus by longitudinal contraction draws the stomach out of
the abdomen into the thorax, there is evidence that the LM of the ureter can
avulse the ureter from the bladder. The mucosa, of course, remains intact, but
the orifice is moved cephalad and the ureters develop bulbous distal extremities
that, when extreme, are remarkably faithful miniatures of a HH.
The treatment rationales are identical except instead of ascribing competence
to a sphincter, the oblique insertion in the bladder muscle is given credit
for ureteral competence against reflux. It seems likely that LM spasm not only
avulses the ureters (intravesicle pressure surely does not do it!) but, by the
same vector resolution, causes reflux. I have seen one ureter that presented
a fair approximation of tertiary contractions.
Sandifer's syndrome and whiplash injuries
Children affected with this condition maintain a posture of extreme dorsiflexion of the cervical spine. This causes sustained and repetitive traction on the esophagus and PEL.(32) All reported cases had HHs.
TABLE 2
Six Cases of Sandifer's syndrome
| Case number | ||||||
| Symptom | 1 | 2 | 3 | 4 | 5 | 6 |
| Hyperextension of neck | X | X | X | X | X | X |
| Reflux | X | X | X | X | X | X |
| Hiatus hernia | X | X | X | X | X | X |
| Vomiting with meals | X | X | X | X | X | X |
| Post-op relief | X | X | X | X | X | X |
| Esophagitis | X | X | X | X | ||
| Aggravated by eating | X | X | ||||
| Anemia | X | X | X | X | X | |
| Elevated fundus | X | X | X | |||
| Esophageal stricture | X | X | ||||
| Dysphagia | X | X | ||||
| Abdominal pain | X | X | ||||
| Age of onset (months) | 20 | 48 | 0 | 60 | ||
Orthopedic surgeons who see cases of whiplash injuries of the cervical spine
report dysphagia as a component of the post-whiplash syndrome. It would seem
that he mechanism of injury is violent dorsiflexion of the cervical spine applying
a sudden force to both the superior and inferior attachments of the esophagus.
I have seen three patients in their 2nd or third decades with a history of whiplash
syndrome who had radiologic signs of rupture of the PEL. This mechanism explains
both the dysphagia (trauma to the superior attachments) and the rupture of the
PEL. The mechanism of injury is identical with that of a tear of the trachea
or main-stem bronchus, but, because it does not lead to life threatening consequences,
it can easily be overlooked.
The power of LMC
It is appropriate to ask, "What kind of force could rupture the PEL? Is it
possible that a thin layer of striated and/or smooth muscle could contract with
enough force to tear this structure?"
Whatever the cause of increased irritability or contractile power of the LM,
there is ample evidence that its tensioning and stretching of the PEL can weaken
it. One has only to observe a vomiting patient at the fluoroscope to be convinced
the power is there. The esophagus contracts instantly, violently retracting
up to a third of the stomach above the diaphragm. Just as quickly, with LM relaxation,
the herniation reduces as the PEL literally snaps it back into place. Seeing
this, even in a young patient or infant, the wonder is that the PEL is not ruptured
in a single vomiting episode.
Earlam(33) cites in detail Herman Boerhaave's graphic description of the patient whose rupture of the esophagus following self-induced vomiting was the first case of Boerhaave's syndrome. At autopsy, the esophagus was found to be completely separated from the stomach!(34)
A more dramatic proof of LM power would be difficult to find.
Although dogs do not naturally develop HHs because of a thick, strong PEL(35)
H. Daintree Johnson(36) demonstrated typical
HHs with cineradiography in dogs by inducing vomiting with apomorphine.
The process is identical in man. Viewing this instant massive spasm(37)
does not engender optimism that a delicate transthoracic Allison repair of the
PEL(38)(39)
will survive postoperative emesis. Raphael et al. reported only a 25%
recurrence rate in 114 Mayo Clinic patients who had postoperative evaluation
after HH repair, however, small recurrences were not counted! They were puzzled
that the patients experienced symptomatic relief even though the HH recurred.
This is not as strange as it might seem. Operative rupture of the PEL, because
it destroys the ability of the LM to open the sphincter, may be an effective
treatment for GER.
Does the stretching result from such violent, episodic LMC or is it a matter of constant tension wearing away stone? I tend to favor the latter - at least for the stretching seen in the so-called slider. If one hangs a weight in the ear lobe, Ubangi-fashion, it will eventually produce elongation. In the same way, a hypertonic LM exerts a constant, lifelong tension on the PEL that must eventually elongate the ligament. One can be sure that this is the case because patients will tell you they feel this tension a major fraction of the day. And this is what they say: "Everything I eat turns to gas!"
The significance of the HH concomitants
A further powerful line of proof is a synergistic one: HH is not an isolated
disorder. It occurs with LERs, reflux, esophagitis, "gas" symptom, tertiary
contractions and non cardiac chest pain unrelated to circular muscle contraction.
The association of multiple abnormalities with each other makes it increasingly
difficult to use different ad hoc explanations for each of them. It
will be shown, for example, that there are separate lines of evidence that LERs
are caused by LMC. Thus, every fact that tends to show that LMC causes the rings
is a further piece of evidence that LMC causes HH because of the invariable
association between LER and HH.
The same is true for the other concomitants of HH mentioned above. If a single
mechanism accounts for LER, GER, HH and TTCs, it is more likely to be correct
than four unrelated hypotheses each of which can only explain one of the four.
The association between HH and Zenker's diverticula
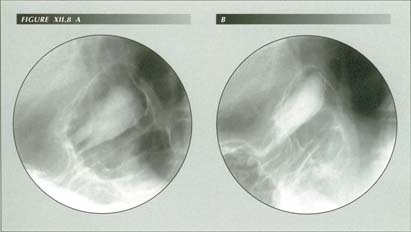
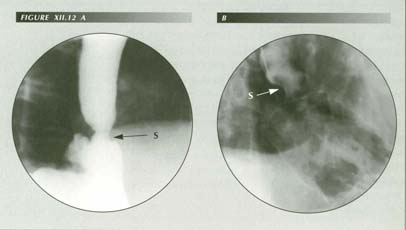
“Watermelon stomach”: Once the PEL ruptures, the stomach remains stationary while the hiatus slides down and up with inspiraion (A) and expiration (B). This can cause stripe-like erosions of the gastric folds as they rub together.
Smiley et al.(41) became interested
in the association and made a special effort to call patients back after surgical
treatment of the diverticulum to reexamine them for HH. Prior to surgery, it
was often difficult to demonstrate a HH because the patient could not swallow
enough barium for an adequate study. Of 32 patients with Zenker's diverticulum,
30 (94%!) also had HHs. After reviewing the literature and evaluating the various
mechanisms proposed to explain Zenker's diverticula, these authors concluded
that GER caused a "dysfunction" of the cricopharyngeus muscle that initiated
diverticulum formation. They were themselves dissatisfied with that formulation.
Reviewing the subject in 1985, Lerut, Leman and Gruwez(42)
concluded the origin of these diverticula remains unknown. As of 1994, the cause
is still "controversial."(43)
As usually happens when two conditions coexist, speculation has centered on
how one causes the other. Seaman(44) states
that "Neuromuscular incoordination . . . is held to be responsible . . . but
the evidence is conflicting." The conflict is between studies showing that the
superior constrictor does not relax normally, that it relaxes normally but closes
too soon, and that it relaxes too late.(45)
With the most current techniques (Arndorfer pneumo-hydraulic capillary infusion
system) Knuff et al. found normal relaxation of the upper esophageal
sphincter (UES) and no evidence of spasm, impaired relaxation ("achalasia")
or incoordination in their nine cases.
Yet one strives in vain to conceive how the three abnormalities could be etiologically
related if increased intra-abdominal pressure or a weak area of the diaphragm
is the cause of HH, low resting sphincter pressure the cause of reflux and neuromuscular
incoordination the cause of Zenker's diverticulum.
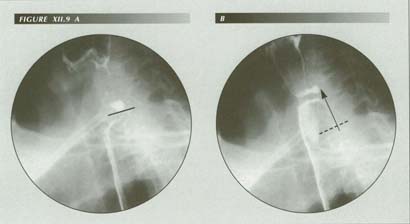
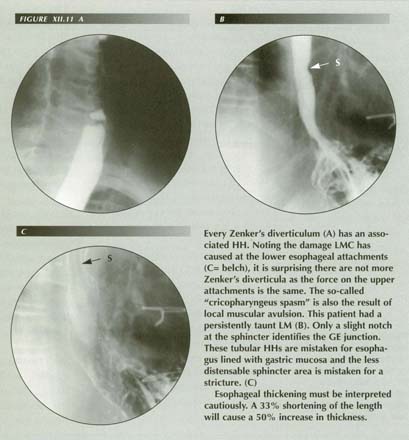
Symptomatic post-cricoid ring with Zenker’s diverticulum: CC: “Food sticks in throat.” Comparing these landmarks with the first rib or a cervical vertebrae shows they have an upward excursion of 2.8 cm at the outset of deglutition. This exerts an abrupt, forceful tug on the esophagus which, transmitted to the PEL, may supply all the force needed to open the sphincter. The sharp tug may also trigger a stretch reflex causing LMC. As is invariably the case with Zenker’s diverticula, the patient also had a HH. The association of the two is due to the circumstance that powerful LMC stretches or disrupts the esophageal attachment at the hypopharynx as well as at the diaphragm.
Actually, there is little evidence of a weak area at the point of origin of
Zenker's diverticula. The hypopharyngeal wall at this point has a double
thickness - the cricopharyngeus and the inferior constrictor of the hypopharynx
overlap. Wilson(46) states, "I have dissected
the posterior wall of the pharynx on many occasions and have always failed to
find anything to suggest a natural triangular area of weakness in this position."
Heuristically, I find this association particularly elegant as each disease provides the clue to the cause of the other and for a bonus solves another puzzle - cricopharyngeal dysphagia.
Cricopharyngeal dysphagia
The deep indentation of the barium column by the cricopharyngeus muscle was
once thought to be due to spasm. Subsequent manometric investigations disproved
this. Mistiming has been incriminated but then disproved.
Cruse et al.(47) investigated the
microscopic pathology in a series of 7 patients ranging from age 1 to 70 who
had a cricopharyngeus myotomy for treatment of dysphagia using tissue obtained
from the myotomy. Twenty post mortem examinations served as controls. The pathologic
findings encountered were death of muscle cells, phagocytosis, replacement fibrosis,
shrunken myotubes, atrophy, regeneration, etc. None of the controls were so
involved. Torres et al.(48) describe
only hypertrophy, but their study was keyed to demonstrating the correlation
between the size of the impression and the size of the muscle and the sections
shown may have been selected to show hypertrophy.
Cricopharyngeus “spasm”:
The force of LM contraction is considerable. Shortening 40% or more of its length, it can tear the lower esophagus from the diaphragm, stretching or avulsing the PEL. A force of equal magnitude and opposite direction is consequently applied ot the hypopharyngeal attachments of the organ. The pathological findings in excised specimens of the so-called “cricopharyngeal bar” are those of old hemorrhage and fibrosis - typical of repeated soft-issue injuries. When the larnx elevates it no longer stretches the upper esophageal sphincter properly giving rise to this appearance. Note that a post-cricoid web is also present causing the marked turbulence (B). This homolog of the “Schatzki ring” further demonstrates the similar mechanics of causation. The patient had heartburn almost daily. Occasional wet spot on his pillow in AM. Lost his teeth at age 32. At fluoroscopy, grade iii esophagitis, grade iv reflux, tertiary contractions, HH and duodenitis, grade iii, were also noted. The p-wave showed impaired cleanup.
Cruse and his associates were left with no hypothesis to account for the damaged
muscle.
The histologic description provided by the Cruse group is typical of the pathology
of repeated episodes of injury with repair and replacement fibrosis seen in
several stages in the same specimen. As with Zenker's diverticulum, once we
are aware of the mischief LMC can create at its nether extremity, we are not
at a loss for an explanation of the injury to the cricopharyngeus muscle. Repeated
tears from vomiting, gagging or simply from long continued tension not only
account for the injury to muscle but for its repeated nature.
Stretching or tearing of the proximal attachments of the esophagus would have
a predictable effect on the upper esophageal sphincter. These structures serve
to resolve the force of the upward displacement that initiates a swallow. The
lateral components of this force open the UES. To the extent this force is late
(with ligamentous stretching) or absent entirely, the difficult of a bolus gaining
entrance to the mouth of the esophagus increases.
This can best be visualized by imagining what would happen if the pharyngeal
attachments of the esophagus were completely severed. Then, when the larynx
rose, the transverse slit-like esophageal lumen would remain a slit and the
bolus would simply overflow it, pooling in the pyriform sinuses and valleculae,
regurgitating into the nasopharynx or being aspirated. In other words, exactly
what happens with cricopharyngeal bars.(49)
One can hope that in 40 years, when and if this information has infiltrated the conventional wisdom, cricopharyngear myotomy will no longer be practiced.
Shortcomings of the increased intra-abdominal pressure hypothesis
This hypothesis - it is more of a default judgement - fails to account for
the morphology of the various types of HH. It gives a false prediction of relative
frequency. It gives no explanation of the association with LERs, reflux and
TTCs and does not account for symptoms.
This lack of understanding has given rise to the situation in which clinicians
complain that radiologists have become too proficient at demonstrating
HHs. The consensus of one symposium was that HHs are only significant (refluxwise)
if they are demonstrated without trying too hard! Yet the association of HH
and reflux is obvious once it is known that they are both due to the same cause
- LMC.
Therapeutic implications
If large hernias are less symptomatic than small ones, is there any point
in making little ones out of big ones? A consensus is emerging that there is
no point in treating a HH per se but that the emphasis should be on
antireflux procedures.(50) Unfortunately, in
many minds "antireflux" still means creating an angle of His. As a result a
fundoplication is by far the most popular surgical approach. Treatment should
be directed at the symptoms of LER, strangulation and reflux. The mere presence
of a HH is no indication for treatment.
Given that there is an indication for surgical intervention, does the Allison
procedure (plastic repair) make sense in the light of the pathogenesis? This
is surely a question that will be debated - radiologists' views on treatment
are seldom embraced by surgeons. However, I have fluoroscoped too many vomiting
patients to have any confidence that a surgical repair of the PEL will survive
even one emesis. Given that the state of the LM is known to be "hyper", the
stress that caused the HH in the first place will frequently cause a postoperative
recurrence. Years ago, when anesthetists were less expert at preventing postoperative
emesis, recurrences were routine. They probably occurred in the recovery room.(51)
On the other hand, the pulldown operations of the original (non-fundoplication) Nissen(52) and Boerema(53) type appear rational. They are far less formidable operations and have a striking benefit. The expedient nature of the operation - a quick fix for patients in poor surgical condition - seems to have tainted it in the eyes of some. Moreover, given the repair philosophy of dealing with hernias in general, pulldown procedures had no rationale. Not surprisingly, they were not considered quite respectable, at least among thoracic surgeons of my acquaintance, and fueled what Earlam calls the trade union debate between thoracic and abdominal surgeons over the preferred approach.
However, if HH is due to the force of LMC, the shoe is on the other foot.
A pulldown procedure not only has a rationale, but the rationale is a correct
one. If traction caused the HH and its concomitants, countertraction is a reasonable
way to treat them. Elongating the esophagus or preventing it from shortening
unduly is a rational way to treat reflux. Shortening a redundant PEL should
only make it worse. Rationally, rupture of the PEL makes sense! It would destroy
the ability of the PEL to open the sphincter. It would prevent Zenker diverticula
and cricopharyngeal tears.
One drawback would be the creation of a iatrogenic Type II HH. Barrett was concerned that the "paraesophageal HHs" would strangulate and expressed a willingness to operate on them. Although in my experience clinicians treat such cases with benign neglect, I have yet to see such a patient get into serious trouble.
SUMMARY
All lines of evidence point to the longitudinal muscle as the cause of HHs.
They can be produced experimentally by provoking LM contraction, either by stimulating
the peripheral end of the transected vagus or by inducing vomiting with apomorphine.
They can be elicited clinically by inducing LMC by forcing the esophagus to
swallow against resistance.
LMC explains the intimate association of HH with LERs, tertiary contractions,
cricopharyngeus spasm, Zenker's diverticulum, non-cardiac chest pain, "gas"
and reflux. It causes all of them.
LMC accounts for the morphologic details of the various HHs and explains their
relative frequency. Sliding HHs differ from other types because, in them, the
PEL is intact whereas it is ruptured or attenuated in the others. LMC cannot
only avulse the inferior attachments of the esophagus to the diaphragm, but
also weaken its attachments to the hypopharynx thus causing hypopharyngeal diverticula
and cricopharyngeal bars.
Terminal anular constriction (A) is not a carcinoma, a stricture or “terminal esophagitis” of Schatzki but a sphincter that cannot efface because of rupture of the PEL (B)
The multiple causes of vomiting, whether it be intestinal flu, food poisoning,
anesthesia, drug reactions and the like, provide all of the trauma required
to produce the appearances seen by the radiologist and surgeon.
Initially, the PEL undergoes elastic elongation and contraction. The elongated
membrane forms a tent-like hood over the retracted fundus. When LMC subsides,
the elastic recoil of the PEL restores appearances to normal. The tent vanishes
and the fundus returns to the abdomen. The process is perceived as a "sliding
HH."
With the passage of time and the repeated insults of life, the PEL loses some
of its elasticity and elongates to permit sliding HHs up to about 7-8 cm to
form. Beyond that, it will not stretch. The next time the patient vomits, the
PEL ruptures. The sliding HH is cured, and a new, generally less annoying syndrome
supervenes - rupture of the PEL. The latter is occasionally marked by a mild
dysphagia due to non-effacement of the sphincter or anaemia due to the mechanical
trauma of rugae rubbing against each other as they pass through the diaphragm
with respiration.
The original limitation on size is now removed so the amount of stomach in
the chest can be much greater. Portions of the omentum are then seen in the
chest. The edge of the diaphragm can be seen notching the greater and lesser
curvatures of the stomach, riding up and down with respiration.
Such HHs occur whether or not the esophagus is shortened by LMC. The fundus
must either telescope over the esophagus producing the familiar "molar tooth"
configuration or push the esophagus to the right. In the latter case, there
will be an acute angle between the esophagus and the fundus. This is usually
cause for misdiagnosing it as a "paraesophageal HH."
A major significance of hiatus "hernias" is their reliable testimony to an
abnormal increased tone of the LM.
A more accurate knowledge of pathogenesis should lead to improved treatment.
Although the term "hernia" is sanctioned by long usage, it is not appropriate.
Elongation of the PEL and rupture of the PEL are the correct designations. A
shorter, etiologic designation would be "esophageal transtraction" or "a gastric
transtract" for sliding HH and "rupture of the PEL" for the others.
For present purposes, however, we are now able to use the insight gained from the analysis of H Hs to take a fresh look at "achalasia" and the various brands of "esophageal motor disorders". The result of this application may be unexpected.
References
Return to Table of Contents
Last Updated July 30 2007 by David PJ Stiennon
1. . Bockus Gastroenterology, Fourth Edition, Vol. 2, Ed. Berk, J. Edward, W.B. Saunders Company, Philadelphia, 1985.
2. . Brombart, Marcel, Clinical Radiology of the Esophagus. John Wright & Sons, Ltd., Bristol, 1961.
3. . Alimentary Tract Roentgenology, Eds. Marguelis, Alexander R. and Burhenne, H. Joachim, C.V. Mosby Company, Saint Louis, 1973.
4. . Diseases of the esophagus. Eds. Cohen, Sidney and Soloway, Roger D., Churchill Livingstone, New York, 1982.
5. . Esophageal function in health and disease. Eds Castell, Donald O. and Johnson, Lawrence F., Elsevier Biomedica, New York, 1983.
6. . In: Esophageal Disorders, Eds. DeMeester, Tom R. and Skinner, David B., Raven Press, New York, 1985.
7. . Postlethwait, R.W., Surgery of the Esophagus, Appleton-Century-Crofts, Norwalk Connecticut, 1986.
8. Yet he later cites a case of his own with a lye stricture which "...literally pulled the stomach into the mediastinum."
9. . Dey, F.L., Gilbert, N.C., Trump, R. and Roskelly, R.C., Reflex shortening of the esophagus in the experimental animal with the production of hiatus hernia. J. Lab. Clin. Med. 31:499-506, 1946.
10. . Kerr, Robert M., Hiatus hernia and mucosal prolapse.
In: The Esophagus, Ed. Castell, Donald O., Little Brown and Company, Boston,
1992.
11. . Webster's New Collegiate Dictionary, G. & C. Merriam Company, Springfield, Massachusetts, 1973.
12. . Dorland's Illustrated Medical Dictionary, 24th Ed., W.B. Saunders Company, Philadelphia.
13. The other is the urinary bladder from which miniature hernia-like outpouchings are produced by traction of the ureter in severe cases of vesicoureteral reflux in children.
14. . Von Bergman, C. and Goldner, M., Functionelle Pathologie, Springer, Berlin, 1932.
15. . Hurst, A.F., Recurrent hernia of the stomach through the hiatus oesophageus of the diaphragm, Guys' Hosp. Rep. 84:43-50, 1934.
16. . Dey et al., op. cit..
17. . Rall, Joseph E., Gilbert, N.C. and Trump, Ruth C., Effect of vagus stimulation on the longitudinal fibers of the stomach and esophagus, Quart. Bull., Northwestern Univ. M. School
19:194, 1945.
18. . Torrance, H. Bruce, Studies on the mechanism of gastro-esophageal regurgitation. J. Roy. Co. Surg. (of Edinberg) 4:54-62, 1957.
19. . Christensen, James and Lund, Gordon F., Esophageal response to distention and electrical stimulation. J. Clin. Invest. 48:408-19, 1969.
20. .Dodds, Wylie J., Current concepts of esophageal motor function: clinical implications for radiology. AJR 128:549-561, 1977.
21. . Dodds, Wylie J., Stewart, E.T., Steff, J.J., et al. Longitudinal esophageal contractions; a possible factor in the genesis of hiatal hernia. Invest. Radiol. 11:375, 1976.
22. .Johnson, H. Daintree, Active and passive opening of the cardia and its relation to the pathogenesis of hiatus hernia. Gut 7:392-401, 1966.
23. . Stiennon, O. Arthur, The "captive bolus" test and the pinchcock at the diaphragm: an esophageal pump and some non-diseases of the esophagus. Am. J. Roentgenol. Tad. Therapy and Nuclear Med. 99:223-32, 1967.
24. . Cannon, W.B., The mechanical factors of digestion, Arnold, London, 1911. Cited by Johnson, H. Daintree, Active and passive opening of the cardia in relation to the pathogenesis of hiatus hernia. Gut 7:392-401, 1966.
25. . Akerlund, A., Hernia diaphragmatica. Hiatus esophagei von Anatomishen und Roentgenologischen Gesichstpunkt. Acta Radiologica 6:3, 1926.
26. There is a fourth type of HH which has been widely studied, but under an entirely different name - the Barrett esophagus.
27. . Barrett, N.R., Hiatus hernia: a review of some controversial points. Brit. J. Surg. 42:231-43, 1954.
28. . Earlam, Richard, Clinical tests of oesophageal function, Grune & Stratton, New York, 1975.
29. . Barrett, N.R., op cit..
30. . Sprafka, Joseph L., Monouchehr, Azad, and Baranofsky, Ivan D., Fate of esophageal hiatus hernia: a clinical and experimental study. Surgery 38:519-24, 1955.
31. . Cameron, Alan J. and Higgins, John A., Linear gastric erosion: a lesion associated with large diaphragmatic hernia and chronic blood loss. Gastroenterology 91:338-42, 1986.
32. For a fuller discussion of Sandifer's syndrome see the section on GER.
33. . Earlam, Richard, op cit..
34. In less complete ruptures and the Mallory-Weiss syndrome the tears are longitudinal.
35. . Eliska, O., Phreno-oesophageal membrane and its role in the development of hiatus hernia. Acta. Anat. 86:137-50, 1973.
36. . Johnson, Daintree, op cit..
37. . Staufer, Herbert M., Akbar, Bonakdar-Pour and Woloshin, Henry J., Brief massive spasm of the distal esophagus greatly increasing gastric herniation documented cineradiographically in a patient with lower esophageal ring. Gastroenterology 38:637-40, 1960.
38. . Allison, P.R., Reflux esophagitis, sliding hiatal hernia and the anatomy of repair. SG&O 92:419-31, 1951.
39. Allison stresses two things he believes to be essential in repair of HH's: 1.) Shortening the PEL by dividing it near its insertion on the esophagus and suturing the proximal edges to the under surface of the diaphragm and 2.) suture of the two sides of the hiatus behind the esophagus with "non-strangulating sutures."
40. . Henderson, R.D., Hanna, W, Marryatt, G. and Kando, M., Cricopharyngeal dysphagia secondary to gastroesophageal reflux: clinical, investigative and pathologic findings. In: Esophageal Disorders, Pathophysiology and Therapy. Eds. DeMeester, Tom R. and Skinner, David B., Raven Press, New York, 1985.
41. . Smiley, T.B., Caves, P.K and Porter, D.C., Relationship between posterior pharyngeal pouch and hiatus hernia. Thorax 25:725-31, 1970.
42. . Lerut, T., Leman, G and Gruwez, J.A., Treatment of pharyngoesophageal diverticulum (Zenker's diverticulum): a comparative study. In: Esophageal Disorders, Pathophysiology and Therapy. Eds. DeMeester, Tom R. and Skinner, David B., Raven Press, New York, 1985.
43. . Rubesin, Stephen E. and Youseun, David M. , Structural abnormalities, In: Gastrointestinal Radiology, Eds., Gore, Richard M., Levine, Mark S. & Laufer, Igor, W.B. Saunders, Philadelphia, 1994.
44. . Seaman, William B. In: Bockus Gastroenterology, Fourth Edition, Vol. 2, Ed. Berk, J. Edward, W.B. Saunders Company, Philadelphia, 1985.
45. . Caves, Philip K., Posterior pharyngeal pouch. Brit. J. Hosp. Med. 8:307-313 September, 1971.
46. . Wilson, C., Pharyngeal diverticula, their cause and treatment. J. Laryngol. & Otol. 76:151-80, 1962.
47. . Cruse, J., Edwards, D.A.W., Smith, J.F., et al., The pathology of cricopharyngeal dysphagia. Histopathology 3:223-32, 1979.
48. . Torres, William E., Clements, James L., Jr., Austin, Garth, et al., Cricopharyngeal muscle hypertrophy:radiologic-anatomic correlation, AJR 142:927-30, 1984.
49. . DeMeester, Tom R., Surgery for esophageal motor disorders. In: The Esophagus, Ed. Castell, Donald O., Little Brown and Company, Boston, 1992.
50. . Skinner, David B., Klementschitsch, Peter, Little, Alex G., DeMeester, Tom, and Belsey, Ronald R.H., Assessment of failed antireflex repairs. In: Esophageal Disorders, Eds. DeMeester, Tom R.
and Skinner, David B., Raven Press, New York, 1985.
51. In accord with the Law of Compensating Errors, that could be the chief merit of the operation. Failure of the suture line should alleviate reflux.
52. . Nissen, R., Gastropexy as the lone procedure in the surgical repair of hiatus hernia. Am. J. Surg. 92:389-92, 1956.
53. . Boerema, M.D., Gastropexia anterior geniculata for sliding hiatus hernia and for cardiospasm, J. Internat. Col. of Surg. 29:533-47, 1957.