The mechanism of mucosal fold formation
Although I am primarily concerned with the muscle of the esophagus, some of
the things to be proved will be derived from the fold pattern of the organ.
A correct understanding of fold formation and its significance is, therefore,
essential.
Historical background
influential textbook. Forssell was impressed that mucosal folds about a cube
of meat in a cadaver stomach seemed to grip the food as though to manipulate
it and theorized that mucosal folds came about by contraction of the muscularis
mucosae.
Forsell's theory was widely accepted and it would be fair to say that it is still unchallenged. As recently as 1983, Eastwood(3)
undoubtedly stated the conventional wisdom when he wrote: "The longitudinal
folds in the lower esophagus are due to contraction of the muscularis mucosae."
On the other hand, Levine and Laufer(4) (1992)
use these fibers to explain transverse folds in the esophagus. Olmstad(5),(6)
echos these views in 1994.
Unfortunately, the autoplastic theory is a hypothesis that leads nowhere. If the theory is correct, no conclusions could be drawn from the fold patterns of the alimentary tract. Fold thickening or thinning could only be interpreted as variations in the activity of the m. mucosae. An increase or decrease in the number of folds would have no particular significance other than suggesting that a different type of m. mucosal activity was present. Fold direction becomes meaningless.(7)
To be sure, radiologists pay little more than lip service to the theory, drawing
diagnostic inferences from fold patterns as their collective experience indicates.
Nevertheless, the discrepancy between theory and practice creates difficulties.
These difficulties are not ameliorated by endoscopists whose methods do not
refute the autoplastic theory. With the organ distended, the enlarged folds
seen by radiologists often were not confirmed by the endoscopist. This could
not help but be embarrassing and inevitably led radiologists to distrust their
own findings and even refuse to draw inferences from fold size or numbers.
This reticence was not lost on the radiological audience. A professor of medicine(8),
speaking as one of a "think tank" of experts on the esophagogastric junction
could say without contradiction by the other members of the symposium that ".
. . . neither [gastritis or esophagitis] is diagnosable radiologically."
Endoscopy also underdiagnoses. A recent study(9) (the endoscopists were unaware it was being done) showed that although endoscopy missed only 17% of histologically verified instances of duodenitis, 68% of the antral gastritis was not diagnosed by inspection. The fact that the stomach is distended for the procedure while the duodenum, presenting no distal barrier to the escape of gas, is less easily distended, explains the different percentages: when an organ is distended, the folds disappear.
Flaws in the autoplastic theory
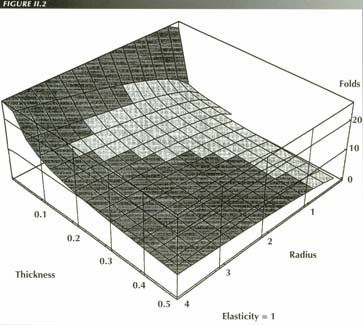
A 3-D Mathematica plot of the fold formula. Without any assumptions, the surface accurately predicts the number of folds that will form when a hollow organ of radius “r” and mucosal thickness “t” contracts. In this plot the elasticity “E” is 1. The surface is little altered overall by smaller values of “E”, but does degenerate as mucosal thickness approaches the radius of the organ
The autoplastic theory, therefore, predicts that esophageal folds will be
exclusively transverse! In fact, of course, esophageal folds are longitudinal
- exactly the opposite of the prediction. If, in unusual circumstances, a transverse
fold does form, we are unable to explain why the usual constraints are in abeyance.
When the stomachs of cats were surgically removed and immediately frozen in liquid nitrogen, sections of the folds showed that the smooth muscle layer of the m. mucosae simply followed the fold parallel to its surface instead of extending directly across the base of the fold bowstring fashion as would be predicted by the autoplastic theory.
One would also have to consider the possibility that folds could form in a
way analogous to the mechanism by which an inchworm folds its body by muscular
contraction. However, this analogy will not hold: the inchworm has muscle layers
on opposite sides of a body 4-6 mm thick. Because the m. mucosae cells
are separated from each other by microns, there is no lever arm that could exert
a folding force.
Finally, it is hardly reasonable to attribute fold formation to a microscopic
muscle layer when there are macroscopic muscle layers that have not
been taken into account.
A demonstration that mucosal folds are caused, not by the muscularis mucosae, but by the muscularis propria has immediate practical consequences. It brings theory into accord with observation. It makes appearances intelligible. It offers predictions that can be verified. It aids in the analysis of new observations. It leads to rejection of the ad hoc assumptions that must be used presently to effect some sort of concordance between autoplastic dogma and the way things look - assumptions that tend to take on a life of their own. Best of all, a correct theory makes gastrointestinal radiology less of an enigma to the student.
A new theory of fold formation
This inescapable fact allows us to set up equations that can be solved analytically to yield a formula that predicts the number of folds that will form with a lumen-obliterating contraction. The derivation is detailed in the Appendix. For practical purposes, the following simplified form of the result is adequate:
 | |
| Where T = the thickness of the mucosa, R = the radius of the organ and E = a decimal fraction for elasticity. Both T and R are measured while the circular muscle is relaxed. |
From the formula, several conclusions can be drawn:
The need to take up the free mucosal surface is both a necessary and sufficient
cause of mucosal folds. Contraction of the muscularis mucosae is a
redundant postulate. The folds would form even if the m. mucosa did
not exist.
The number of folds is proportional to the resting radius. That is, the larger
the organ, ceteris paribus, the more folds it should have.
Fold number is inversely proportional to the thickness of the mucosa.

Esophageal folds: Normal folds measure 1 mm or less and one can count 5 or 6 of them they are caused by the circular muscle, not the m. mucosa that is also longitudinal. There are no transverse folds unless, for one reason or another, the esophagus can shorten with LMC

Severe esophagitis, grade iii: 2 folds occupy the entire width of the relaxed body.
Pathologic states that affect the thickness and elasticity of the mucosa should reduce the number of folds while increasing their thickness. There is a reciprocal relationship between fold number and fold size - obviously, the fewer the folds, the larger they must be to encompass the width of the organ. In many ways, however, it is desirable to use fold number rather than fold size diagnostically. Although counting folds is not always easy, it is a great deal easier to quantify fold number than absolute size. The great variety of imaging media affects the measured size of the folds, borders are not always definite and magnification by the divergent beam varies a good deal.
Qualitatively, the course of fold formation can be reconstructed as follows: As the gut contracts, no folds need form until the radius of the hollow organ is reduced beyond the ability of the mucosal elasticity to take up the slack. Thereafter, the surface is thrown into folds as the increasingly redundant lining membrane adjusts to the diminishing circumference of the lumen. Finally, when the tone of the contracted organ reduces the area of the lumen to zero, the maximum number of folds will be present.
Due to the fine-structure of the cellular and stromal elements of the mucosa,
it does not, except under stress, depart much from a fixed configuration. When
partially distended, the fold pattern is still traceable. Folds always form
in the same places as the living tissue "takes a set" if the lumen is normally
collapsed.
There may well be and probably are, interrelationships among the variables,
but this does not affect the validity of the formula. It is likely, for example,
that inflammatory disease affects both the thickness and the elasticity of the
mucosa.
In deriving the formula, it was assumed that, when the circular muscle contracts, as much mucosa is squeezed into a given cross section as is squeezed out. There are rare instances where this assumption is not valid and a progressively tighter squeeze diminishes the fold size as tissue is extruded from the area of interest. In nature, folds are often compound. No attempt was made to take this into account in the derivation, yet the prediction of fold number is extremely accurate.
Clinical correlation
Having developed a new theory to account for mucosal fold formation, it is
appropriate to see how well it does at explaining or predicting the familiar
clinical-radiological appearances.

Longitudinal muscle contraction causes transmverse folds: The widely distended bowel could be due to paralasis or distention. Folds cannot form unless the lumen is obliterated. Numerous transverse folds, misnamed valvulae conniventes, prove that the LM is contracting and thus distinguish mechanical obstruction from paralytic ileus in which atony of the m. propria prevents any fold formation
The reverse is also true. Mucosal atrophy - best visualized in the stomach
- leads to many "cigarette paper" folds as would be predicted by the formula.
Similar folds may occur in ulcerative colitis.
The larger organs have more folds, e.g., the stomach vs. the esophagus. Very
small organs, exhibit no folds at all - the elasticity is enough to take up
all the slack as the distended state is little different from the contracted
state. This is also predicted analytically from the derived formula as follows:
If the thickness of the mucosa equals the radius of the organ, the numerator of the fold formula becomes zero.
 |
therefore |
 |
That is, when the radius of the lumen is equal to the mucosal thickness, no folds will form. This is approximately true, of course, for all small tubular organs - the ureters, the eustachian tubes the fallopian tubes, the vas deferens - which, as predicted, have no longitudinal folds. |
Even in the vascular system, the appearances are in accord with the prediction of our model: it predicts no folds at all! The difference in diameter between the contracted and distended states is such that elasticity can take up any redundancy that develops in diastole. Unlike the gut, the lumen of a blood vessel is not obliterated on contraction. Hence, any redundancy of the endothelium on contraction is minimal and the elasticity is enough to absorb it.
What has been said applies specifically to folds caused by contraction of the
circular layer of the muscularis propria. It will be noted that the
folds formed by circular muscle are orthogonal to the plane of the circular
muscle fibers, i.e., are longitudinal or parallel to the long axis of the organ.
Transverse folds with eventration of the diaphragm: Although the patient did not have an elongated PEL, eventration of the left leaf of the diaphagm
We can generalize and state categorically that mucosal folds are orthogonal
to the muscularis propria fibers that produce them.
In the esophagus, our present area of interest, this new theory has immediate
application. The fold pattern of the esophagus supports the theory and the theory
explains the pattern. Unlike the rest of the gut, the esophagus has the singularity
that it normally has no slack. Because it is attached to the skull via the pharynx
above and to the diaphragm below, its ability to shorten with LMC is limited.
Consequently, in the normal organ, there are no transverse mucosal folds. Lacking
such constraints, the circular muscle can produce longitudinal folds. If, due
to a hiatus hernia, rupture of the phreno-esophageal ligament or marked kyphosis,
the esophagus can shorten with LMC, then transverse folds - rings or webs -
do form.
Looking at this interesting situation teleologically one can get a clue as to the function of the m. mucosae. It is appropriate to the function of the esophagus that it does not have transverse folds. No useful purpose served by the delay such folds would produce in transport through the organ. Folds such as webs and LERs produce dysphagia.
Lengthwise arrangement of submucosal muscle fibers also affects the other parameter
of the fold equation, elasticity. The greater the elasticity, the fewer
the folds. Smooth muscle fibers in the submucosa increase the elasticity
of the mucosa and prevents fold formation. If the m. mucosae could
produce transverse folds in the normal esophagus, it would do so. That the esophagus
must shorten about 15% before transverse folds appear gives us a rough estimate
of .85 for the numerical value of the elasticity, E, of esophageal mucosa.
An understanding of the mechanism of fold formation will be useful in the study of the esophagus because we can work the theory both ways and use the mucosal fold pattern to monitor continuously which component of the muscularis propria is contracted.
A compelling example of the utility of the theory is in the differential diagnosis
of mechanical and paralytic ileus. In both conditions the small bowel is markedly
dilated. This does not necessarily mean that the circular muscle is paralyzed
or otherwise defective. The dilatation is occasioned by mere distention. However,
the presence of transverse (Kerckring) folds in the typical "coiled spring"
appearance signifies LMC. Correctly, we can infer that if the LM is contracting,
the ileus is not paralytic.
Both radiologist and physiologist know when the circular muscle is contracting because it reduces the caliber of the lumen, produces longitudinal folds, compresses a balloon or raises intraluminal pressure. In sharp contrast, none of these indispensable signs is seen with LMC. The ability to identify which component layer of the muscular wall is contracting fluoroscopically is very useful, particularly with the LM of the esophagus.
SUMMARY
When a hollow organ contracts enough to obliterate its lumen, the mucosal lining
becomes redundant. This redundancy is accommodated by the formation of folds.
It can be shown analytically that the number of folds is a function of the resting
size of the organ and the thickness and elasticity of the mucosa. The direction
of the folds is orthogonal to the direction of the muscle fibers of the m.
propria that cause them.
Unlike the autoplastic theory, the present analysis generates testable predictions
that are in exact correspondence with the radiological findings in hollow tubular
organs, particularly the gut.
Once it is realized that transverse fold formation implies LMC, a new range of physiological observations becomes possible.
References
Last Updated July 26, 2007 by David PJ Stiennon
1. 1.Forssell, G., Normale und pathologische reliefbilder des schleimhaut: ein uberblick uber die autoplastic des digestionskanales, Verhand 1. d. Gesellsch. f. Verdauungsskr., 7 Tagung, 199-219, 1927.
2. 2.Templeton, Frederick. E., X-ray Examination of the Stomach, the University of Chicago Press, Chicago, 1968.
3. 3.Eastwood, Gregory L., Esophagitis and its consequences In Esophageal function in health and disease, Eds Castell, D.O. and Johnson, Lawrence F., Elsevier Biomedical, New York, 1983.
4. 4.Levine, Marc and Laufer, Igor, Esophagus. In: Double Contrast Gastrointestinal Radiology, 2nd edition, W.B. Saunders, 1992.
5. 5.Olmsted, William W. In: Gastrointestinal Radiology, Gore, Richard M., Levine, Mark S. & Laufer, Igor, Eds., W.B. Saunders, Philadelphia, 1994.
6. 6.Olmsted, Wlliam, AJR 127:423-8.
7. By the same token, survival of the autoplastic theory can be attributed to the paucity of verifiable predictions it gives. Without these, it is difficult to prove it false. There is, however, a school of thought that holds that if there is no way a theory can be demonstrated false, it is false.
8. 8.Palmer, Eddy D., Hemorrhage at the esophagogastric junction. In: The esophagogastric junction. Proceedings of a symposium held in Las Croabas, Puerto Rico, Eds. Katz, David and Hoffman, Fredrick. Excerpta Medica, Princeton, 1971.
9. 9. Johnstone, B.J. and Reed, P.I. and Ali, A.H., Correlation between endoscopic appearances and histological diagnosis of antral and duodenal inflammation. (Abstract) Gastroenterology 90:1480, 1986.
10. . Geboes, K and Desmet, V., Histology of the esophagus. Front. Gastrointest. Res. 3:1-17, 1978
11. . Schumacher, S., Handbuch der Microskopischen Anatomie des Menchen, J. Springer Verlag, Berlin, 1927.

