Gas/bloat and the physiology of belching
"For the clinician, the bęte noir of the symptoms referable
to the digestive tract is 'gas'."(1) Patients
can assure themselves of instant rejection by complaining, "Everything I eat
turns to gas!" Unfortunately, "gas" and the equivalent symptom of "bloat" is
the most common of all gastrointestinal complaints.(2)
Efforts to correlate the "gas" symptom with objective evidence of gas have
been futile. Although physicians have " . . . been well indoctrinated that swallowed
air is the cause of alimentary tract gas.",(3)
they often see patients with flat bellies and gasless radiographs who paradoxically
complain, "I feel as though I were going to explode!" On the other hand, a patient
may have visible abdominal distention without complaining of gas. Patients with
ascites, pneumoperitoneum or extreme obesity seem oddly immune to the complaint
of bloating. On the other hand, patients with mechanical bowel obstruction and
a genuine gas problem, complain of cramps, not gas.
This puzzle of "gas without gas" has motivated many studies. Although these
have yielded exact data on the production, composition, absorption, elimination,
and clinical correlations of intestinal gas, they only deepen the mystery. Lasser
and associates,(4) for example, using a sophisticated
isotope washout technique, found that 12 patients with this complaint averaged
23 ml less intestinal gas (177 ml) than 10 normal controls (200 ml).
In extreme cases, the patient may habitually perform alternate Mueller and
Valsalva maneuvers to fill and empty the esophagus with gas (as in esophageal
speech) to provoke eructation of gas from the stomach in the belief this will
afford relief. In an occasional patient, this can get completely out of hand.
The false eructation may become a social liability - an outrageous, gross habit
that the patient is apparently unable or unwilling to control.
Most such patients are eventually referred for radiologic examination where,
aside from demonstrating of aerophagia(5) if
it is extreme, the results have given no clue to the cause of this bizarre performance.
Various theories are (6)offered. Nevertheless,
none carry any conviction or suggest an experimental test that would either
confirm or refute them. Roth(7) relates belching
to aerophagia, splenic flexure syndrome, "magenblase syndrome" and neurosis,
considering it only in the context of the excessive belching of aerophagia.
He lists aerophagia as caused by most of the disorders of the upper GI tract.
He speculates that the habit forms because the ". . . patient experienced some
relief of a distress with the eructation of air . . . and thus deliberately
induces belching by aerophagia to secure that relief again."
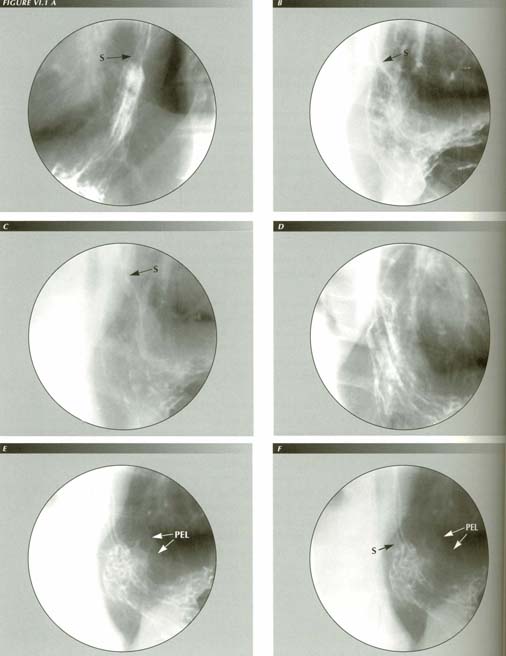
FIGURE VI.1 A-F - Belching produces a HH. Over the course of a lifetime, belching gagging, rapid swallowing, and vomiting generally stretch the PEL beyond its elasic limits - a limit that is also decreaasing with age.
Earlam(10) lists some quantitative information:
the gastric gas bubble is less than 50 ml of air 2-3 ml are swallowed with each
bolus; 1,000 swallows/day (70/hr while awake, 7/hr while asleep) would result
in total ingestion of 2.0 to 3.5 liters of gas per day. He also reports that
the average audible belch contains 20-80 ml and requires simultaneous contraction
of the abdominal musculature and relaxation of the sphincter.
One need not consult standard references to become acquainted with the mechanics of belching. Self-observation will go a long way. Thus one finds he unconsciously leans forward, head up, neck extended. The larynx ascends as in swallowing and gas is released. The forward inclination of the thorax is particularly noticeable if one is restrained by the shoulder strap of a seat-belt.(11) Unfortunately, this introspection gives no clue to what is going on at the lower end of the esophagus. It would be much better to study the process fluoroscopically.
Inducing a belch at fluoroscopy
Chance fluoroscopic observation of a belch initially aroused my interest in
the problem. Thereafter, I was frustrated by the infrequency with which I could
study the process further. Chance observations were infrequent and when they
did occur, one seldom had the area of interest in the field of view, good wall
coating, cine camera on, etc. One cannot just wait for a belch to happen - fluoro
time will run out with the examination uncompleted.
Belch: LMC jerks the stomach into the chest to the end of the tethering PEL
LMC induction of eructation
There appear to be two factors involved in the success of this maneuver, neither
of them the amount of air in the stomach:
1. The gas or bloat symptom. Such patients yield the bulk of the positive responses.
2. The amount of water employed. Using 180-250 cc of water and rocking the
patient back and forth to slosh it about the fundus seems to increase the yield.
With this technique, there were many opportunities not only to secure sequence
spot and cine films but also to ask patients whether the sensation experienced
during longitudinal muscle contraction (LMC) was the same as the sensation they
were calling "gas."
The first visible warning of an impending belch is a slight conical tenting
of the otherwise hemispherical outline of the fundus or the formation of a hooded
appearance of the fundic mucosal folds.(12)
This may vanish or become more pronounced. If the latter, a hiatus hernia, if
present, becomes drawn upward to the full length of the tethering phrenoesophageal
ligament. The whorls of mucosal folds in the fundus then straighten and point
to the gastroesophageal junction and that junction assumes the shape of a trumpet
bell or, more accurately, an alpenhorn. The diaphragm is tented and, as a result,
loses its sharp outline because the central ray of the beam passes through the
tent rather than grazing the diaphragmatic dome.
This bell shape is the shape of an elastic membrane under traction. The greater
the force applied to the center of the membrane, the more acute the apex angle
of the cone of tensed membrane. The perihiatal region of the diaphragm itself
may also be tented upward. These changes are manifestations of a LM contraction
that, in extreme cases, may shorten the esophagus 36% or more.
The sphincter then opens and stomach gas instantly inflates the esophagus.
If the voluntarily controlled superior constrictor opens, gas escapes into the
pharynx, is eructated and the fundus collapses. If not, an en masse
contraction of the circular muscle and/or a peristaltic wave forces gas back
into the stomach.
In this way, a striking event in patients who belched under fluoroscopic study
was a preparatory strong contraction of the LM (LMC). Questioning the
patients as it occurred established that the gas/bloat sensation was simultaneous
with the signs of LMC.
This portion of the act of belching, unlike gagging or vomiting, is quite
deliberate and usually occupies several seconds. LMC may be sustained for a
considerable time if, for any reason, the superior sphincter does not open.
As much as 8-10 seconds is not unusual and in an exceptional instance it may
be sustained 30 seconds or longer allowing ample time to question the patient.
Sphincter release does not follow every preparatory LMC. The LMC may simply
subside or there may be a partial subsidence followed by contraction leading
to an almost rhythmic ebb and flow of tension on the GE junction marked by varying
shape of the trumpet bell. The greater the force applied to the center of the
membrane, the more acute the angle of the apex of the cone formed by the stretched
membrane.
On cine films in such cases, one can see the sphincter margins alternately approaching and receding from each other as though prepared for an instant closure whenever some very delicate balance of forces is destabilized. This process is a clear and convincing demonstration that the LM opens the sphincter: the shorter the LM, the higher the GE junction and the more patent the sphincter.
Gas/bloat is a misinterpretation of LMC
Sometimes, the conscious control of belching can be dramatic as in the following
case:
11/4/66 H.D. 45151/M-426 Fluoroscopic note: There was considerable aerophagia
and a large amount of gas accumulated in the stomach. A "hiatus hernia" was
present that was ideally provoked by having the patient belch, a feat at which
he was unusually proficient and could perform on command. This produced shortening
and elevation of the esophagus, evoked the HH and was associated with a descent
of the diaphragm resulting in a violent jerking motion of the stomach back and
forth through the hiatus. Cine films confirmed and showed free cardio-esophageal
reflux.
The tension noted during LMC is perceived at the conscious level as gas although
the patient's description of the sensation may be quite variable. Most had trouble
defining the sensation, but such expressions as "It feels full.", "Kind of pulling.",
"Like a pressure.", or "Bloated." were used. When the cardia tents, if a leading
question, "Does it feel as though you were going to belch?" is asked, the response
is usually an unequivocal "Yes." From there it is a small step to the conclusion
that the sensation preceding a belch is what patients mean by "gas" and similar
vague fornulations.
Patients often expressed surprise that I knew they were about to belch or that
I could see a belch although they had eructated silently and politely! The uniformly
positive identification of LMC with the gas sensation left no doubt about the
cause of this mysterious symptom. The identification was convincing after relatively
few cases because the patient could identify the symptom with the event as
it happened. That is, he did not have the sensation throughout the examination,
but at the exact time I observed traction on the gastric fundus.
The LM tension has many interpretations other than gas and bloat as in the
following case.
LM051846: This 50 year old male truck driver complained almost constantly of
the sensation of a mass "about the size of a large potato" beneath the right
diaphragm. Occasional heartburn. Ultrasonography revealed a normal gallbladder
and minimal evidence of fatty infiltration of liver. Upper GI demonstrated grade
ii reflux (asymptomatic), grade ii duodenitis and antral gastritis. When the
fundus tented after the dC maneuver he was surprised I was able to tell exactly
when he was having the mass sensation.
He was given a 10 mgm capsule of Nifedipine with instructions to chew and swallow
it the next time the symptom was severe. He reported back within the hour, "I
didn't take it on the drive home because I wasn't sure what it would do to me,
but I had complete relief of the symptom within minutes of swallowing the pill.
I feel completely relaxed."
Gas, or better, LM tension is a symptom because there is a condition in which
LM tension is hyper - "longitonia" if you will. The LM contracts, increasing
its tension on the diaphragm, even when there is no physiologic need for it
to do so. It does not require the stimulus of gas distention of the stomach
to exert traction on the PEL. A degree of traction great enough to force the
sphincter by vector resolution will also tension the diaphragm. For this reason,
patients with reflux usually also complain of gas/bloat.
The reason patients misinterpret LM tension on the diaphragm is that LM contraction
is an event that frequently precedes eructation of gas. It is independent of
whether or not there is actually gas in the stomach. This is why the gas sensation
does not correlate with how much gas in the stomach. It is purely a function
of LM tension.
As was noted earlier, extension of the neck is a belch-facilitating maneuver.
This is true because extending the neck applies tension to the esophagus and
may also produce a stretch reflex.
From the point of view of patient care, I believe the identification of the
"gas" symptom with LM tension is of value. At a minimum, efforts to decrease
gas formation or to adsorb gas on activated charcoal (It has been done!) are
futile. Pharmacologic efforts to reduce LM tone would be more rational.
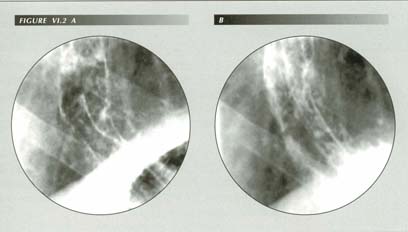
Gas-bloat with LMT. Male 56, pyrosis, bloat, nocturnal laryngospasm, lost teeth at 26. An uneffaced sphincter serves for measurement of LMC. Note shortening from A to B. The esophagus was constantly shortened. This causes traction on the diaphagm producing the “gas-bloat” symptom. This patient also has an enalarged lingual tonsil, gr. 2 vallecular sign and the p-wave was ineffectual.
There seems at least a lay consensus that certain foods produce gas. Seed catalogs advertize burpless varieties of cucumbers. Is it possible that such foods contain an active ingredient that heightens LM tone?
Belching and mass contraction of the longitudinal muscle
Like the LMC of nausea, pyrosis and vomiting, there is no peristalsis associated
with the LMC of belching except for a post-belch cleanup wave. The force of
LMC can be gauged by the size of the conical tent; the higher and thinner the
tent, the greater the traction that is being applied to it.
It is noteworthy that, although in peristalsis LM and CM contraction are precisely
integrated, in en masse contraction they are can be independent. In
pathologic circumstances - particularly diffuse esophageal spasm - simultaneous
LM and CM en masse contractions also can occur. In all of these
cases, it is striking how the esophagus, to play its many roles, coordinates
its several functional elements in sharply different ways.
Because it enables us to correlate pressure relationships in the esophagus
with the events just described, it is useful to review the phenomena McNally,
Kelly and Ingelfinger(13) recorded from the
2-dimensional viewpoint of the manometer. They found that insufflation of the
stomach with air via catheter raised the intragastric pressure to 5-7 mm Hg.
Within the 200-1600 cc range, intragastric pressure was independent of how much
air was introduced, suggesting that distention rather than pressure is a stimulus
to belching.
Manometrically, the escape of air from the stomach into the esophagus was signaled
by a sudden equalization of gastric and esophageal pressures [i.e., sphincter
release]. In cases where it was possible to record the intrasphincteric pressure,
it was found that it could be maintained at values equal to the intragastric
pressure for periods of 14-110 seconds before the escape of gastric gas into
the esophagus. In two cases ". . . reflux occurred 88 and 96 seconds respectively
after intragastric pressures had exceeded those recorded in the sphincter
zone." [Emphasis added, i.e., pressure gradients were not sufficient to open
sphincter.] The authors were puzzled that ". . . . no. . . . correlation between
increased gastroesophageal pressure gradients and the appearance of simple reflux
was noted."
In a later study, Sigmund and McNally(14) found
a gradual reduction in sphincter pressure preceding a belch induced by essence
of peppermint, a carminativet. Perceptively, they drew a significant conclusion:
"The gradual decrease in intrasphincteric pressure suggests an active relaxation
of the sphincter rather than a passive one, secondary to the increased gastric
pressure forcefully distending the sphincter." [Emphasis added.] That active
agent, however, is the LM not intragastric pressure.
Both radiologic and manometric techniques demonstrate that release of gas via
the superior constrictor may be delayed for many seconds or inhibited entirely.
Kahrilas et al.(15) using manometric
techniques found that the upper esophageal sphincter (UES) released gas 1-10
seconds after the common cavity effect [gastric pressure = esophageal pressure]
that denotes release of the LES. The reflex controlling its relaxation could
distinguish between refluxing fluid and gas, probably by sensing the spatial
and temporal characteristics of release of gas into the body of the esophagus.
As it was unimpaired by mucosal anesthesia these authors were able to exclude
a mucosal pH receptor.
Because the sphincter is closed in these preliminary stages of belching, the
state of the circular muscle of the body of the esophagus in not seen directly.
However, the instant the sphincter opens, the body of the esophagus balloons
to its full diameter. From this, we can be certain that the circular muscle
behind the sphincter is relaxed at the time of sphincter release. This establishes
that LM contraction is not accompanied by CM contraction in belching.
The esophageal lumen collapses as the gas leaves via the superior constrictor. Fluoroscopically, I find it impossible to decide whether this collapse is due to an en mass contraction of the circular muscle or to a momentary Valsalva maneuver that occurs simultaneously with the belch. The latter could force gas from the esophagus even without circular muscle contraction. There is manometric evidence that, like the LM, the circular muscle is not restricted to one mode of contraction. McNally et al. interpreted a simultaneous spike in the tracing from a catheter placed in the colon as an indication that a brief Valsalva maneuver was occurring. This, however, is subject to another interpretation as will be seen in the next chapter.
Belching and the CD receptor
We have seen that a sustained forceful LM contraction inetiates sphincter opening
and allows the escape of gas from the stomach. What terminates the egress of
gastric contents? Several lines of evidence indicate that then acid/pepsin contacts
a fundic recptor LM contraction is inhibited and the sphincter, released from
its dilating force, closes.
Often, a belch is not a single event. It may be one of a sequences of eructations
of which the first is usually the largest (noisiest) followed by cleanup secondary
or tertiary burps. This is particularly the case in infants. It seems that if
they are going to spit up feeding, it occurs on the secondary burp.
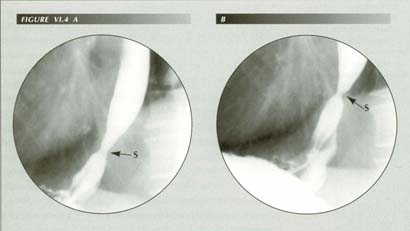
Belch: (A) Before, (B) after. Although the release of air from the stomach may be explosive, unless the superior constrictor releases, the esophagus may remain air-distended for 8-24 seconds, affording an excellent opportunity to note the traction effects of LMC and their correlation wih the opening of the sphincter. Barium is dilute from he dC test which has turned off the CD receptor that acts as a guardian of the gate to prevent reflx when submerged in acid/pepsin. The trumpet shape explains the orad directed wedge shape of Mallory-Weiss tears.
These observations only confirm what everyone knows from personal observation
- that normally, even when the stomach is full after a meal, gas can be released
from the stomach very forcefully without regurgitating fluids. Parents burping
infants discover this fact several times a day. Mechanistically, the problem
is to learn how the sphincter (or better, the LM that is holding it
open) knows that in a few milliseconds the esophagus is going to be doused with
gastric contents and finds out in time to do something about it.
The experiments of Dougherty et al.(16)
demonstrated the elaborate arrangements ruminants have evolved to prevent reflux
of gastric fluids while allowing free escape of gas. The reticuloruminal fold
acts as a dam to prevent fluid from reaching the esophageal orifice. Gas, of
course, can travel over the dam to exit the stomach. Less elaborate, but nonetheless
effective measures perform the same function in man.
By the constraints placed upon it, the receptor for this reflex closure should
be a chemoreceptor. Yet, if one postulates such a sensor, the rapidity of its
transmission to the motor arm of the reflex is difficult to square with the
time it takes for a chemical to diffuse to the depth of the sensor and through
any mucus coating it. On the other hand, gastric irritation from certain foods
may cause increased mucus production that, by coating the receptor, puts the
watchdog to sleep with resulting reflux and heartburn. Such a mechanism would
account for the latent period between a dietary indiscretion and the onset of
heartburn.
The alternative to a chemoreceptor is some system of sensors that continually
monitor the shape of the stomach - a possibility, perhaps, as the shape of a
stomach partially filled with air would, for the same volume of contents, be
different from one filled entirely with fluid.
There are, however, objections to the latter hypothesis. For one thing, the analogy to the CD receptor is too strong. It will be recalled that the nerve network demonstrated by Dougherty and his co-workers is near the esophageal orifice. This is more in keeping with a chemoreceptor activated when contacted by gastric contents than it is with shape sensing. The latter would require a diffusely distributed net of sensors not localized to this specific region at all.
Surgical causes of the gas/bloat symptom
The gas/bloat symptom is inseparable from the act of belching because the LM
tension that produces sphincter release of necessity also exerts traction upon
the diaphragm. The symptom is produced whether or not sphincter release is achieved.
We have seen that the association of the sensation of diaphragmatic tension
with belching causes misinterpretation of this tension with its normal result
- an eructation of gas.
Without really intending to do so, surgeons will often perform experiments
for us on a scale so vast they have great statistical significance. One way
of surgically producing tension on the diaphragm is to pull the GE junction
down below the diaphragm and suture the stomach around it so it will not retract
to its normal position. By thus "taking a tuck" in the esophagus, a more or
less continuous pull on the diaphragm is created as the hypertonic LM tries
to pull the plicated fundus through the hiatus. Thus, the gas bloat syndrome
which may persist for many years after a Nissen fundoplication. An Angelchik
prosthesis often produces the same effect(17)
for the same reason.
Infantile colic
Before leaving the subject, there is one aspect of belching that probably deserves
discussion - infantile colic. The colicky baby screams, apparently for no reason,
as the parent walks the floor wondering what to do to relieve the child's evident
misery. The screams seem senseless and different in kind from those of a hungry
baby. The infant may be soothed by again feeding it but soon it is having another
attack of colic.
Careful mothers learn never to put the baby back in its crib before it has
been burped, but this is not always a solution. It is a trial to the parent
because the burp may not come until it is nearly time for the next feeding.
Perhaps because of its association with difficulty in burping, the implicit
assumption is that colic is due to the excessive air that, failing a satisfactory
burp, must be passed through the GI tract. However, radiologists, who see many
infant chest and abdomen radiographs, know that non-colicy infants normally
have quantities of gas in the small and large bowel. If gas leaves the stomach,
there is nothing to stop it being eliminated as flatus. As adults, we are aware
that it is no problem to pass any required amount of gas and that it is not
painful to do so. Why should it be any different for infants?
When we think of a bowel cramp, we think of a sustained contraction of the
circular muscle, because all of the bowel cramps with which we are
familiar are circular muscle cramps. Circular muscle spasm can be seen with
the fluoroscope, e.g., the cramping pain often associated with barium enemas
in a patient with a spastic sigmoid, the pylorospasm noted with delayed gastric
emptying - or felt by the examiner as with the broom handle descending colon
palpated in patients with spastic colons. We are just not accustomed to seeing
LM spasm in the bowel, much less to palpating it.
This produces a typical clinical impasse: a set of symptoms leads the physician
to expect a corresponding set of objective findings. The expected findings do
not appear. Conclusion: "No disease; over-anxious mother."
Yet colic is too common, too real and too disruptive to the lives of young parents to be dismissed in this fashion. The same parents may alternate children with and without colic. To me it seems far more probable, because of its association with burping problems, that infantile colic may be the simply the pediatric equivalent of bloat. Unfortunately, infants cannot describe their symptoms, but it would add weight to this supposition if the symptom responded to medication as did my patient's "gas" symptoms.
SUMMARY
The mechanism at the lower esophagus must be able to permit eructation of air
while denying egress to gastric fluid contents. Two elements are involved:
1.) The CD reflex, which inhibits LMC when activated, must be turned off.
2.) The sphincter must be opened by vector resolution of the force of LMC.
These two mechanisms account for the perfection of control of this physiologic
function.
"Gas," a symptom that is the bane of the clinician, is due to LMC. LMC applies
tension to the diaphragm via the PEL. Because the resulting sensation normally
precedes a belch, it is identified at the conscious level as a sensation of
gas, bloating or epigastric fullness. It can be seen radiologically as a tenting
of the cardia, especially if a modification of the usual deCarvalho test technique
is used to induce belching by turning off the receptor for the CD reflex.
Postoperative gas/bloat is due to surgically tensioning the esophagus by fundoplication
or insertion of a prosthesis. The problem of the colicky baby is discussed in
the light of the relation of LMC to belching. It seems that "baby bloat" would
explain the phenomena better than current rationales.
As would be anticipated, patients who have a slack, elongated esophagus as in achalasia are unable to belch(18) Vagal cooling abolishes transient sphincter relaxation in dogs by abolishing LMC. The deliberate eructations I have described in this chapter, although most easily studied fluoroscopically are not the most common. There is a second method of sphincter release, alone or in cooperation with LMC. This will be discussed in more detail in the following chapter.
References
Last Updated July 27, 2007 by David PJ Stiennon
1. 1. Roth, J.L.A In: Bockus Gastroenterology, Fourth Edition, Vol. 2, Ed. Berk, J.E., WB Saunders Company, Philadelphia, 1985.
2. 2. Lasser, R.B., Bond, J.H. and Levitt, MD, The role of intestinal gas in functional abdominal pain. N Engl J Med 1975; 293:524-6.
3. 3. Anon., Gas. Editorial, N Engl J Med 1969; 281:164-5.
4. 4. Lasser, et al., op cit..
5. A misnomer. Little if any of the air aspirated into the esophagus reaches the stomach.
6. 5. Bockus, H.L., Gastroenterology, 2nd Ed., W.B. Saunders, Philadelphia, 1963.
7. 6. Roth, J.L.A. In Bockus, H.L., Gastroenterology, 2nd Ed., W.B. Saunders, Philadelphia, 1963.
8. 7. Bockus, H.L., op cit.
9. A maneuver that stretches the esophagus.
10. 8. Earlam, Richard, Clinical tests of oesophageal function, Grune & Stratton, New York, 1975.
11. Perhaps this is one factor in citizen resistance to wearing them!
12. This hood is the mysterious "image en burnous" of Jutras, et al.
13. 9. McNally, Edmund F., Kelly, J. Edward and Ingelfinger, Franz J., Gastroenterology 46: 245-9, 1964.
14. 10. Sigmund, Charles J. and McNally, Edmund F., The action of a carminative on the lower esophageal sphincter. Gastroenterology 56:13-18, 1969.
15. 11. Kahrilas, P.J., Dodds, W.J., Dent, J.B., Wyman, J.B., Hogan, W.J. and Arndorfer, R.C., Upper esophageal sphincter function during belching. Gastroenterology 91:133-40, 1986.
16. 12. See the chapter on the Cannon-Dougherty reflux for references
17. 13.Burhenne et al., op cit.
18. 14. Holloway, R.H., Dent, J. and Wyman, J.B., Impairment of belch reflex in achalasia: evidence for neural mediation of transient lower esophageal sphincter relaxation. (Abstract) Gastroenterology 91:1055, 1986.
